Tinnitus and Ringing in the Ears from Medications: What to Know
 Dec, 18 2025
Dec, 18 2025
Medication Ototoxicity Risk Checker
Check Medication Risk for Tinnitus
Enter the name of any medication to check its potential to cause tinnitus (ringing in the ears).
Have you started a new medication and suddenly noticed a ringing, buzzing, or hissing in your ears? You’re not alone. Tinnitus - that persistent sound with no external source - can be triggered or worsened by many common drugs. It’s not just a minor annoyance. For some, it becomes a constant companion that disrupts sleep, focus, and even mental health. The good news? In many cases, it’s reversible. The key is knowing which medications to watch for, how to spot the signs early, and what to do next.
What Exactly Is Medication-Induced Tinnitus?
Tinnitus isn’t a disease. It’s a symptom. And when it’s caused by a drug, it’s called ototoxicity. That means the medication is damaging parts of your inner ear or the nerve that sends sound signals to your brain. This damage can cause ringing, roaring, clicking, or even a high-pitched whistle - usually in both ears. It might show up within hours of taking a new pill, or it could creep in slowly over weeks.
Over 600 prescription and over-the-counter drugs are known to cause or worsen tinnitus, according to recent clinical reviews. That includes everything from painkillers and antibiotics to antidepressants and cancer drugs. The scary part? Many people don’t realize their tinnitus is drug-related. They assume it’s just aging, stress, or noise exposure. But if the ringing started after you began a new medication, that’s a red flag.
Which Medications Are Most Likely to Cause Ringing in the Ears?
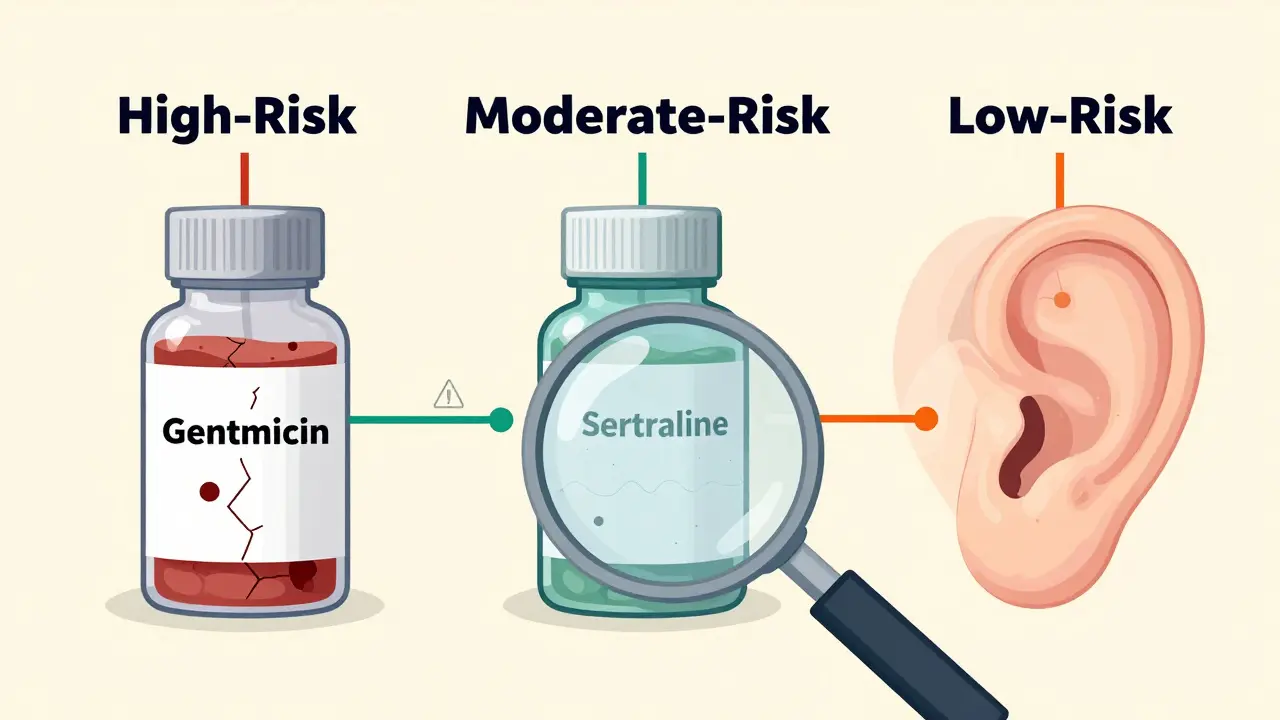
Not all drugs carry the same risk. Some are far more dangerous than others. Here’s a breakdown of the most common culprits, ranked by risk level:
- High-risk drugs: These can cause permanent hearing damage. Includes aminoglycoside antibiotics like gentamicin and tobramycin (especially when given IV), platinum-based chemotherapy like cisplatin (up to 70% of patients develop hearing issues), and loop diuretics like furosemide (Lasix) used for heart failure or kidney problems.
- Moderate-risk drugs: Often reversible if caught early. Includes aspirin - but only at very high doses (4,000 mg or more daily). Modern headache doses (325-650 mg) rarely cause issues. Also includes isotretinoin (Accutane) for acne, which affects about 5% of users.
- Low-risk drugs: Tinnitus is rare. Includes most antidepressants like sertraline (Zoloft) or fluoxetine (Prozac), affecting less than 1% of users. Also includes beta blockers - but only some, like carvedilol. Aténolol doesn’t seem to cause it.
One surprising fact: NSAIDs like ibuprofen and naproxen can trigger tinnitus, especially at high doses. One Reddit user reported ringing within 48 hours of taking 800 mg of ibuprofen three times a day for a toothache. The sound faded within a week after stopping. That’s a classic case of temporary ototoxicity.
Why Do Some Drugs Hurt Your Ears?
The exact science isn’t fully understood, but researchers believe ototoxic drugs interfere with the tiny hair cells in your cochlea - the part of your inner ear that turns sound waves into electrical signals. These cells don’t regenerate. Once they’re damaged, the signal to your brain gets distorted, and you hear phantom sounds.
Some drugs also affect blood flow to the inner ear or disrupt the balance of electrolytes like potassium and sodium, which are critical for nerve function. That’s why kidney function matters. If your kidneys can’t clear the drug properly, it builds up and increases your risk. That’s why doctors monitor blood levels of drugs like gentamicin - to keep doses safe.
Is It Permanent? How Long Does It Last?
This is the biggest question for most people. The answer: it depends.
- Reversible: About 60% of cases clear up within days to weeks after stopping the drug. This includes tinnitus from NSAIDs, high-dose aspirin, quinine (used for malaria), and even some antidepressants.
- Potentially permanent: Aminoglycosides and cisplatin can cause irreversible damage. Even after you stop the drug, the ringing may stick around. That’s why doctors test hearing before and during treatment for these drugs.
- Delayed onset: Some people don’t notice tinnitus until weeks or even months after starting a drug. This is common with antidepressants and benzodiazepines. It’s not always the drug itself - sometimes it’s the withdrawal. Stopping sertraline suddenly, for example, has been linked to new-onset tinnitus in case reports.
Most people who develop drug-induced tinnitus notice it within the first two weeks. If you’ve been on a medication for six months and suddenly hear ringing, it’s less likely to be the drug - but still possible.
What Should You Do If You Notice Ringing After Starting a New Drug?
DO NOT stop your medication on your own. That’s dangerous. Some drugs - like blood pressure meds or antidepressants - need to be tapered slowly. Stopping abruptly can cause serious side effects.
Instead, do this:
- Write it down. Note when the ringing started, what it sounds like, and whether it’s constant or comes and goes.
- Check your meds. Look up the drug’s side effects on a trusted site like the FDA’s database or your pharmacy’s info sheet. Many list tinnitus as a possible side effect.
- Call your doctor. Don’t wait. Say: “I started [drug name] two weeks ago, and now I have constant ringing in my ears. Could this be related?”
Your doctor might:
- Switch you to a different drug with lower ototoxic risk
- Lower your dose
- Order a hearing test to check for damage
- Monitor your kidney function if you’re on a high-risk drug
Many people are surprised to learn their doctor can often find an equally effective alternative. For example, if you’re on a high-dose NSAID for arthritis, switching to a COX-2 inhibitor or a non-NSAID pain reliever might solve the problem.
Can You Prevent Medication-Induced Tinnitus?
Yes - but it takes awareness and action.
- Ask before you start. When a new medication is prescribed, ask: “Can this cause ringing in the ears or hearing loss?”
- Get baseline hearing tested. If you’re starting cisplatin, gentamicin, or another high-risk drug, ask for an audiogram before treatment begins. That way, doctors can track changes.
- Don’t mix high-risk drugs. Taking multiple ototoxic drugs at once (like aspirin + furosemide) increases risk dramatically.
- Monitor kidney health. Poor kidney function means drugs stay in your system longer. Stay hydrated and get regular blood tests if you’re on long-term ototoxic meds.
- Know your sensitivity. A small number of people are unusually sensitive to aspirin - they get tinnitus even at low doses. If you’ve had this happen before, avoid aspirin and tell your doctor.

What If the Tinnitus Won’t Go Away?
If the ringing sticks around after you’ve stopped the drug, it’s not your fault. You did everything right. Now it’s about managing it.
Studies show that sound therapy (using white noise machines or soft background music) and cognitive behavioral therapy (CBT) help 60-70% of people cope better. These don’t cure tinnitus, but they help your brain stop noticing it as much. Many people report sleeping better and feeling less anxious within weeks.
There’s no magic pill to make it vanish - yet. But research is moving fast. The NIH is funding $12.5 million in studies to find drugs that protect the ear from ototoxic damage without reducing the medicine’s effectiveness. Genetic tests are also being developed to identify people at higher risk before they even start treatment.
Bottom Line: Don’t Panic - But Don’t Ignore It
Medication-induced tinnitus is more common than most people think. But it’s also one of the most treatable forms of tinnitus. The key is catching it early. If you notice new or worsening ringing after starting a new drug, talk to your doctor. Don’t wait. Don’t assume it’s harmless. And never stop your meds without professional advice.
Many people go years thinking their tinnitus is just part of life - until they realize it started after a prescription they forgot about. You have the power to change that. Know your meds. Listen to your ears. And speak up.
Can aspirin cause ringing in the ears?
Yes - but only at very high doses, usually above 4,000 mg per day. That’s far more than the 325-650 mg used for headaches or heart health. At those normal doses, tinnitus is very unlikely. However, a small number of people are unusually sensitive and may experience ringing even at low doses. If you’ve had this happen before, avoid aspirin and talk to your doctor about alternatives.
Do antidepressants cause tinnitus?
Tinnitus is a rare side effect of antidepressants, affecting less than 1% of users. Some SSRIs like sertraline (Zoloft) and fluoxetine (Prozac) have been linked to tinnitus in case reports - both when starting the drug and when stopping it suddenly. If you notice ringing after starting or stopping an antidepressant, tell your doctor. They may adjust your dose or switch medications, but never stop on your own.
Is medication-induced tinnitus permanent?
It depends on the drug. About 60% of cases are reversible and fade within days to weeks after stopping the medication. However, drugs like gentamicin and cisplatin can cause permanent damage, even after you stop taking them. That’s why hearing tests before and during treatment are critical for high-risk drugs.
How long after starting a drug does tinnitus appear?
Most people notice ringing within the first two weeks of starting the drug. But delayed onset is possible - especially with antidepressants, benzodiazepines, or chemotherapy drugs. In some cases, tinnitus appears after months of use or even after stopping the medication. If you’re unsure, track when symptoms began and share that with your doctor.
Should I stop my medication if I get tinnitus?
No. Never stop a prescribed medication without talking to your doctor first. Some drugs need to be tapered slowly to avoid dangerous withdrawal effects. Instead, document your symptoms and contact your prescriber. They can assess whether the drug is the cause and help you switch to a safer alternative if needed.
Can hearing tests detect medication-induced tinnitus?
Yes. An audiogram (hearing test) can show if you’ve lost sensitivity to certain frequencies - a sign of early ototoxic damage. Doctors often test hearing before starting high-risk drugs like cisplatin or gentamicin, then repeat tests every 1-2 weeks during treatment. If changes are detected, they can adjust your dose or switch medications before damage becomes permanent.
What’s Next?
If you’re currently on a medication and experiencing tinnitus, schedule a call with your doctor this week. Bring your list of all meds - including supplements and OTC painkillers. Ask about alternatives and whether a hearing test is recommended.
If you’ve already had tinnitus from a drug and it’s resolved, great. But remember: if you ever need that same drug again, you’re at higher risk. Tell every new provider about your history.
And if you’re starting a new treatment - especially for cancer, infection, or chronic pain - ask the big question: “Could this affect my hearing?” That simple step could save you from months of ringing in your ears.

Frank Drewery
December 19, 2025 AT 18:15I started hearing this high-pitched whine after taking ibuprofen for my back pain. Thought it was just stress until I read this. Stopped the pills and it faded in 5 days. So glad I didn’t ignore it.
Don’t brush off ear stuff - your ears are way more sensitive than you think.
Anna Sedervay
December 20, 2025 AT 17:43One must consider the broader pharmacological context. The ototoxic potential of NSAIDs is grossly underreported in mainstream medical literature due to pharmaceutical lobbying. The FDA’s adverse event database is a farce - only 1% of cases are documented. One must question the integrity of the entire system.
And yet, the cochlear hair cells - those delicate, irreplaceable structures - remain the true silent victims. This is not medicine. This is chemical negligence.
Monte Pareek
December 22, 2025 AT 03:40Listen up. If you're on anything strong like chemo or antibiotics and you hear ringing - don't wait. Don't google it for three weeks. Call your doc tomorrow. I've seen too many people lose their hearing because they thought 'it'll go away' - it doesn't always.
Get a baseline audiogram before starting high-risk meds. Ask for it. Demand it. Your ears are not replaceable.
And if you're on aspirin for heart health - don't panic. 325 mg is fine. It's the 2000 mg doses people crush for headaches that wreck their ears. Know your dose. Know your risk. Stay smart.
Kelly Mulder
December 23, 2025 AT 03:03It is utterly irresponsible that OTC pain relievers are sold without mandatory ototoxicity warnings. The FDA has failed the public. This is not a ‘side effect’ - it is a documented, preventable neurological injury. People are being poisoned by Advil. And no one talks about it. Why? Because profits outweigh patients. The system is broken.
Tim Goodfellow
December 23, 2025 AT 10:17Man I had this wild ringing after my first round of azithromycin - thought I was going crazy. Turned out it was the drug. Stopped it, got a hearing test, and boom - nothing permanent. But man, the first week was hell. I started listening to rain sounds on loop just to drown it out. Now I tell everyone I know: if your ears start buzzing after a new pill - don’t be cool about it. Speak up. It’s not ‘just tinnitus’ - it’s your body screaming.
Elaine Douglass
December 24, 2025 AT 10:03I’ve had tinnitus for years and I swear it got worse when I started sertraline. My doctor said it was unlikely but I asked for a switch anyway. Now I’m on bupropion and the noise is way quieter. I’m so glad I didn’t just suffer in silence. You’re not being dramatic - your ears matter.
Takeysha Turnquest
December 26, 2025 AT 09:19They told us the world was flat. They told us smoking was safe. They told us thalidomide wouldn’t hurt babies. Now they tell us ibuprofen is harmless. But the ringing? The ringing is the truth screaming through the noise. Your ears hear what your mind refuses to believe. The drugs are not healing you - they are rewriting your reality. And they don’t care. They never do.
Alex Curran
December 27, 2025 AT 01:07My uncle took furosemide for heart failure and got tinnitus after two weeks. Doc said it was temporary. Three months later he still hears it. Got a hearing test - permanent damage. Now he uses hearing aids and white noise machines. Point is - don’t assume it’ll go away. Get tested early. Even if your doc says it’s rare. Better safe than sorry.
Allison Pannabekcer
December 27, 2025 AT 13:58I want to say thank you to everyone who’s shared their stories here. This is the kind of info that saves people from years of suffering. I’ve had tinnitus since my teens and it’s been a lonely road. But knowing it can be drug-induced - and reversible - gives me hope. If you’re reading this and you’re scared - you’re not alone. Talk to your doctor. Bring this article. Ask for help. You deserve to hear the world clearly.
Alana Koerts
December 29, 2025 AT 02:58Everyone’s acting like this is news. Newsflash - it’s in the drug inserts. You just don’t read them. You swallow pills like candy and then cry when your ears ring. You think doctors are out to get you? No. You’re just lazy. Read the damn label. It’s right there. ‘Tinnitus: possible side effect.’ You didn’t need this article. You needed to open the bottle.
Nicole Rutherford
December 30, 2025 AT 08:31You think you’re the only one? Everyone’s got tinnitus. Everyone’s on something. You think your ibuprofen is safe? Your coffee? Your vitamin D? Your ‘natural’ supplements? The world is poisoning you and you’re too busy scrolling to notice. You think this is about pills? It’s about control. They want you to be anxious. They want you to hear the noise. So you keep buying more drugs.
Mark Able
December 31, 2025 AT 22:34Wait so if I take aspirin for a headache and my ears ring - I just stop? What if I have a heart condition? Do I just stop my meds and risk a stroke? This article is irresponsible. You can’t just flip-flop on prescriptions like that. You need a doctor. Not Reddit. Not some guy on the internet. You need a professional. Stop panicking. Talk to your doctor. Not the comment section.
Marsha Jentzsch
January 1, 2026 AT 04:50I’ve had this ringing for 3 years… I just thought it was stress… But then I realized… I started Zoloft… and I started hearing it… and I didn’t tell anyone… because I was ashamed… I thought I was weak… I thought I was imagining it… I’m so mad at myself… I should’ve spoken up… I’m so sorry… I just want it to stop…
Janelle Moore
January 1, 2026 AT 12:08They’re hiding this. They know. The FDA knows. The drug companies know. That’s why they don’t put big warning labels on Advil. Because if people knew, they’d stop buying. And then they’d lose billions. This isn’t medicine. It’s a money machine. And your ears are just collateral damage. You think your doctor cares? They get paid by the system. They don’t want you to stop your meds. They want you to stay sick. Wake up.
Monte Pareek
January 1, 2026 AT 12:15Replying to the guy who said ‘just read the label’ - yeah that’s great if you’re a pharmacist with a PhD. Most people don’t even know what ‘ototoxic’ means. And the labels? They’re printed in 6-point font. You need a magnifying glass and a flashlight. That’s not informed consent. That’s a loophole. And if you’re on 5 different meds? You’re not reading 50 pages of tiny print. You’re just trying to feel better. So don’t blame the patient. Fix the system.