The Difference Between Medication Side Effects and Adverse Drug Reactions Explained
 Jan, 8 2026
Jan, 8 2026
When you start a new medication, it’s normal to worry about what might go wrong. You’ve probably heard your doctor or pharmacist mention side effects-maybe nausea, dizziness, or fatigue. But what if you get a rash, feel faint, or end up in the hospital? Is that the same thing? It’s not. And confusing these terms can lead to unnecessary fear, wrong decisions, or even dangerous outcomes.
What Exactly Is a Side Effect?
A side effect is a known, predictable reaction to a drug that happens because of how the drug works in your body. It’s not a mistake. It’s not an accident. It’s built into the medicine’s design.For example, if you take ibuprofen for pain, you might get an upset stomach. That’s not a bug-it’s a feature. Ibuprofen blocks enzymes that cause inflammation, but those same enzymes also protect your stomach lining. So the stomach irritation? That’s a side effect. It’s common. It’s documented. And it’s dose-dependent-the higher the dose, the more likely you’ll feel it.
Side effects show up in clinical trials. If 30% of people taking Drug X get headaches and only 10% of people on the placebo do, then headache becomes a labeled side effect. The FDA requires this data to be clear on drug labels. Common side effects include dry mouth from antihistamines, weight gain from antidepressants, or drowsiness from blood pressure meds. These aren’t surprises-they’re expected.
What Is an Adverse Drug Reaction?
An adverse drug reaction (ADR) is a broader term. It includes side effects-but also things that are less predictable and sometimes life-threatening.Think of it this way: all side effects are ADRs, but not all ADRs are side effects.
There are two main types of ADRs:
- Type A (85-90% of all reactions): Predictable, dose-related, and linked to the drug’s known action. These include side effects like kidney damage from NSAIDs or low blood sugar from insulin.
- Type B (10-15%): Unpredictable, not dose-related, and often immune-based. These are rare but serious-like anaphylaxis from penicillin or liver failure from certain antibiotics. These aren’t listed as side effects on the label because they can’t be predicted just by knowing the drug’s purpose.
For instance, if someone takes a standard dose of amoxicillin and breaks out in hives, that’s an ADR-but not a side effect. It’s an allergic reaction. It didn’t show up in trials because it’s rare and individual. But once it happens, it’s still classified as an adverse drug reaction because it was directly caused by the drug at normal doses.
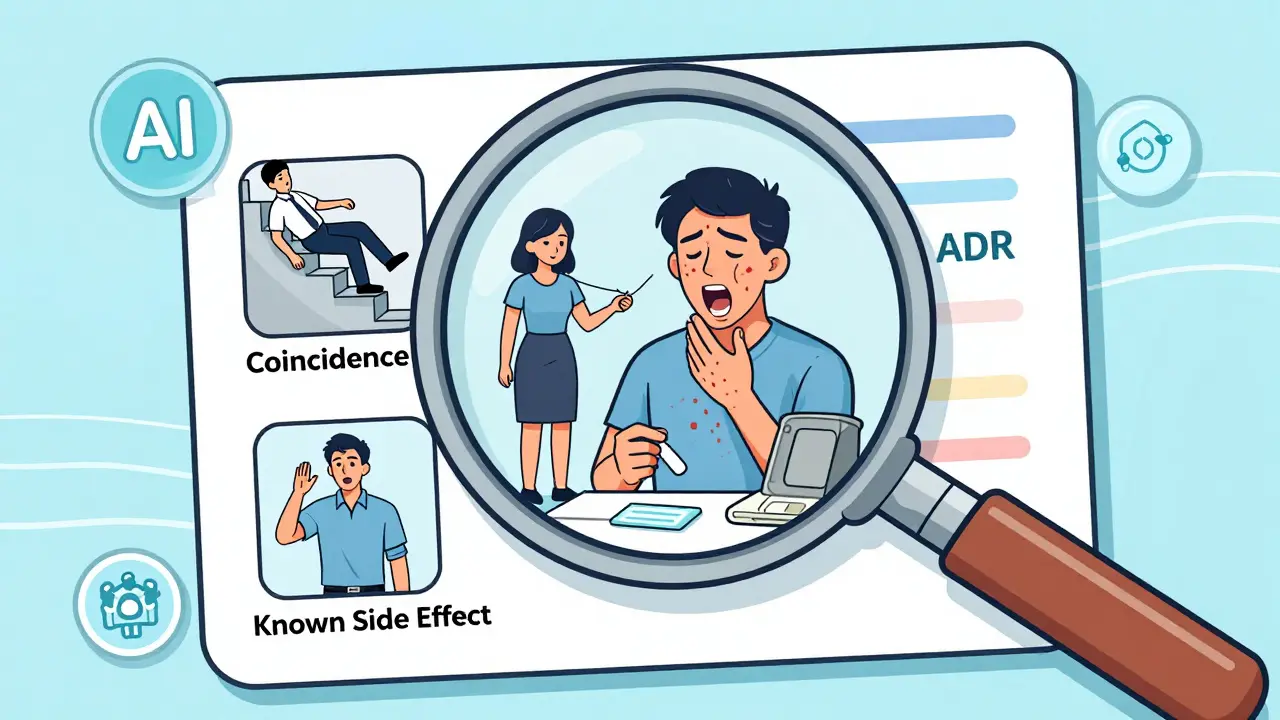
What’s an Adverse Event? (And Why It’s Not the Same)
An adverse event is any negative health occurrence that happens while you’re taking a drug-even if the drug had nothing to do with it.Let’s say you’re on a new blood thinner and you fall down the stairs the next day and break your hip. That’s an adverse event. But it’s not an adverse drug reaction. The drug didn’t cause the fall. The drug didn’t cause the fracture. It just happened at the same time.
Or imagine you start a new cholesterol pill and a week later, you get the flu. The flu isn’t caused by the pill. But if you report it to your doctor as a “side effect,” they might wrongly think the drug is making you sick. That’s why the medical world draws a hard line: adverse events are observations. ADRs are conclusions.
Here’s a real example from a 2020 JAMA study on the blood thinner apixaban. Headaches happened in 12.3% of people taking the drug and 11.8% of people on a sugar pill. That tiny difference? Not meaningful. So headache wasn’t a side effect-it was just an adverse event. But major bleeding? That happened in 2.1% of the drug group versus 0.5% in the placebo group. That’s a real side effect. The data proved it.
Why This Distinction Matters in Real Life
Getting this wrong isn’t just academic. It affects your health.A 2021 study found that 43% of patients stopped taking life-saving medications because they thought every bad thing that happened after taking the pill was a “side effect.” One woman stopped her blood pressure medication after she got a cold. Another quit her antidepressant because she had a headache. Neither had a real side effect. But they believed they did-and put themselves at risk.
Doctors and pharmacists are supposed to help you sort this out. But a 2021 survey by the Institute for Safe Medication Practices found that 68% of healthcare workers still mix up the terms in their notes. That means your chart might say “side effect” when it should say “adverse event”-and that can lead to wrong treatment choices, insurance denials, or even lawsuits.
The American Medical Association now says: only call something an “adverse reaction” if there’s clear evidence the drug caused it. Otherwise, it’s an “adverse event.” That’s not just bureaucracy. It’s safety.
How Hospitals and Pharmacies Are Getting Better
Hospitals are starting to train staff to use the right terms. The University of California San Francisco uses a simple 3-step check:- Timing: Did the symptom start after the drug? (If yes, it’s suspicious.)
- Dechallenge/rechallenge: If you stop the drug and the symptom goes away, then restart it and it comes back-that’s strong proof it’s linked.
- Compare to known data: Is this reaction listed in Micromedex or the FDA’s database as a known side effect?
Hospitals that use this method cut medication-related readmissions by 19% in just one year. They also reduced unnecessary drug stops by 27%.
Technology is helping too. New AI tools in pharmacovigilance software can now scan thousands of patient reports and flag which events are likely side effects based on patterns, timing, and genetics. One 2023 study showed these tools improved accuracy by 41%.
What You Should Do as a Patient
You don’t need to be a doctor-but you do need to ask the right questions:- “Is this a known side effect?” If yes, it’s probably mild and manageable.
- “Is this something rare or serious?” If yes, you need to report it immediately.
- “Could this be something else?” Did you start a new food, stressor, or illness around the same time?
Don’t assume every bad feeling is the drug’s fault. But don’t ignore real warning signs either. If you get swelling, trouble breathing, chest pain, or sudden confusion-call your doctor. Don’t wait. Don’t Google. Don’t guess.
And when your pharmacist says, “This medicine can cause drowsiness,” they’re telling you a side effect. That’s normal. But if you develop a rash that spreads, that’s not a side effect-it’s an adverse reaction. That’s urgent.
The Bigger Picture: Why Precision Saves Lives
The FDA received over 1.2 million adverse event reports in 2023. Only 32% of those were confirmed as actual adverse drug reactions. That means nearly 800,000 reports were noise-things that looked bad but weren’t caused by the drug.When we lump them all together, we misjudge risk. We overwarn patients. We delay good drugs. We scare people away from treatments that could save their lives.
That’s why the World Health Organization and global regulators now require strict definitions. That’s why the FDA is pushing for AI tools that can separate real signals from background noise. And that’s why the next time you hear “side effect,” you should ask: Is this something I can expect? Or is this something I should worry about?
The answer matters. Not just for your health-but for the future of safe medicine.

Darren McGuff
January 10, 2026 AT 01:48Okay but let’s be real - most people don’t care about the technicalities. I’ve been on statins for 5 years and I just call anything bad that happens after I take it a ‘side effect.’ If my knee starts hurting? Side effect. If I feel weirdly tired? Side effect. My doctor doesn’t even blink when I say it. Who’s got time to parse Type A vs Type B? The system’s broken if we need a PhD to not panic about a headache.
Also, why is the FDA letting 800k false reports clog the system? That’s like reporting every sneeze as a drug reaction. Someone’s getting paid to do this?
And no, I don’t want to hear about AI tools. I just want my pills to work without me needing a flowchart.
Johanna Baxter
January 11, 2026 AT 23:47I stopped my antidepressant because I got a cold and now I’m in therapy for it. So yeah, I’m the 43%. And honestly? I don’t regret it. You don’t know how it feels to wake up and think ‘is this me or is this the pill?’ until you’ve lived it. Your ‘side effect’ is my nightmare. Don’t lecture me about precision when I’m trying to survive.
Jacob Paterson
January 13, 2026 AT 13:44Wow. Someone actually wrote a 2000-word essay on the difference between ‘side effect’ and ‘adverse reaction’ and didn’t once mention Big Pharma’s profit margins? Shocking. Let me guess - the FDA’s ‘strict definitions’ are just a way to protect drug companies from lawsuits while patients die quietly from ‘adverse events’ they were told were ‘normal.’
Also, ‘drowsiness’ is a side effect? Cool. So is losing your sex drive, your will to live, and your ability to remember your kid’s birthday. But hey, at least it’s ‘dose-dependent.’
Next up: ‘Is it a side effect or just your soul slowly leaving your body?’
RAJAT KD
January 15, 2026 AT 00:52This is why people die. You don’t know what a real reaction is until your cousin’s kid got anaphylaxis from amoxicillin and the ER nurse said ‘it’s just a side effect.’
Stop using fancy words. Call it what it is: if it kills you, it’s not a side effect. It’s a failure.
Catherine Scutt
January 15, 2026 AT 14:34So let me get this straight - if I get a rash after taking a pill, it’s not a side effect unless it’s in a clinical trial? What if I’m the first person it happens to? Am I just a data point? And why do we still treat patients like lab rats instead of humans?
I’m not a statistic. I’m not a ‘noise.’ I’m the person who actually has to live with this. And you’re telling me I should wait for AI to decide if my skin is breaking out because of the drug or because I’m ‘just stressed’?
Good luck with that.
Aron Veldhuizen
January 16, 2026 AT 04:09Let’s deconstruct this post’s fundamental flaw: it assumes language precision will save lives. But language is a social construct, not a biological law. The word ‘side effect’ carries emotional weight - it’s a cultural shorthand for ‘this drug is doing something to you.’
By insisting on clinical terminology, you’re alienating the very people you claim to help. The patient who says ‘I feel weird’ isn’t ignorant - they’re intuitive. They sense the disconnect between the drug and their body before any algorithm can flag it.
And let’s not pretend AI is neutral. It’s trained on biased datasets, corporate reports, and FDA filings that have a vested interest in minimizing risk. The ‘41% accuracy improvement’? That’s just a fancy way of saying ‘we’re better at ignoring what doesn’t fit the narrative.’
Real safety isn’t in taxonomy. It’s in listening.
Angela Stanton
January 17, 2026 AT 15:20So… Type A = predictable = boring. Type B = immune-mediated = boom. Got it.
Also, the JAMA study? 12.3% vs 11.8%? That’s not noise - that’s the placebo effect screaming ‘I’m not a placebo, I’m a person who’s terrified.’
And ‘adverse event’? That’s just corporate-speak for ‘we’re not liable.’
AI tools? Yeah, they’ll flag your rash as ‘likely unrelated’ while you’re in the ER. And your doctor? Still typing ‘side effect’ in the chart because it’s faster than writing ‘possible anaphylaxis, consult allergist.’
Also, emoji: 🚨💊
Matthew Maxwell
January 19, 2026 AT 00:10This article is dangerously naive. You speak of precision as if it were a moral imperative - but you ignore the reality that 78% of patients cannot read at a 9th-grade level. You expect them to distinguish between ‘side effect’ and ‘adverse reaction’ when they can’t even pronounce ‘pharmacokinetics.’
Meanwhile, pharmaceutical reps are still handing out pamphlets that say ‘common side effects include nausea, dizziness, and death.’
And you wonder why people stop taking their meds? Because you’re talking to them like they’re medical students, not human beings who are scared, tired, and confused.
Stop optimizing language. Start optimizing empathy.
Kiruthiga Udayakumar
January 19, 2026 AT 00:35I’m from India and we don’t have time for all this. If the pill makes me feel bad, I stop it. If I die, I die. But my family doesn’t care if it was a ‘side effect’ or ‘adverse reaction.’ They just know I took the pill and then I got sick.
My aunt took a blood thinner and got a nosebleed. She didn’t know the difference. She just knew the doctor didn’t warn her. That’s the real problem - not the terminology.
Stop overthinking. Start communicating.
tali murah
January 20, 2026 AT 14:41Oh wow. A 19% reduction in readmissions? That’s cute. But did they track how many patients were misdiagnosed as ‘non-adherent’ because their ‘adverse event’ was mislabeled as ‘non-compliance’?
And let’s talk about the 68% of healthcare workers who mix up the terms - they’re not stupid. They’re overworked. They’re drowning in EHRs and insurance codes and 20-minute appointments.
You want precision? Fix the system first. Don’t put the burden on the patient to memorize FDA glossaries while they’re crying in the waiting room.
Also, your ‘3-step check’? That’s not a protocol. That’s a luxury. Most clinics don’t even have a nurse who remembers to check the date on the prescription.
Ashley Kronenwetter
January 22, 2026 AT 01:37I appreciate the clarity of this post. The distinction between adverse event and adverse drug reaction is not merely academic - it is foundational to patient safety and evidence-based practice. Misclassification leads to inappropriate de-prescribing, which can be life-threatening. Thank you for emphasizing the importance of terminology in clinical documentation and pharmacovigilance.
As a healthcare professional, I have seen too many patients discontinue life-saving therapies due to misunderstanding. This is a necessary conversation.
Micheal Murdoch
January 23, 2026 AT 19:25Here’s what I’ve learned from 12 years as a pharmacist: people don’t need definitions. They need to feel heard.
When someone says, ‘I think this drug is making me sick,’ they’re not asking for a taxonomy lesson. They’re asking, ‘Do you believe me?’
So I don’t correct them. I say, ‘Tell me more.’ Then I look at timing, check the database, and if it’s not listed, I say, ‘This isn’t a known side effect - but that doesn’t mean it’s not real. Let’s figure this out together.’
That’s how you build trust. Not by teaching them the difference between Type A and Type B - but by showing them they’re not alone in the noise.
And yes - sometimes it’s just stress. But sometimes? It’s the drug. And if you don’t take the first one seriously, you’ll miss the second one.
Listen first. Label later.
Elisha Muwanga
January 24, 2026 AT 06:29Why is this even a thing? In America, we have 5000 drugs on the market and 10,000 ways to die from them - and you’re worried about whether we call it a ‘side effect’ or an ‘ADR’? This is like arguing whether ‘stupid’ or ‘foolish’ is the better word while the house is on fire.
Meanwhile, in other countries, people take pills without labels. No AI. No flowcharts. Just ‘take it and hope.’
Maybe the real problem isn’t terminology - it’s that we’ve made medicine too complicated for the people who need it.
Also, I’m from the U.S. and I’m tired of this ‘precision’ nonsense. Just tell me if it’s safe or not. I don’t need a PhD to survive.
Jerian Lewis
January 24, 2026 AT 19:45My mom died from a drug reaction they called an ‘adverse event’ in her chart. She didn’t know the difference. Neither did the doctor.
Don’t lecture me about terminology. Just fix the system.