Stomach Ache & Weight Loss: Understanding the Connection
 Sep, 29 2025
Sep, 29 2025
Stomach Pain & Weight Loss Calculator
This interactive tool estimates how much weight you might lose due to stomach pain based on your daily discomfort level and eating habits.
Ever notice that a lingering stomach ache seems to make the numbers on the scale drop? You’re not imagining it - there’s a real physiological link between abdominal discomfort and weight loss. This article breaks down why that happens, which conditions are most likely to cause it, and what you can do to stop the cycle before it turns into a health crisis.
Quick Take
- Stomach pain can suppress appetite, lower calorie intake and boost stress hormones.
- Common culprits include gastritis, peptic ulcers, IBS and infections.
- Sudden or severe weight loss may signal a deeper problem like cancer or malabsorption.
- Managing pain with diet tweaks, stress reduction and medical treatment usually stabilises weight.
- Track symptoms, food logs and seek professional advice if you lose more than 5% of body weight in a month.
First, let’s define the two key players.
Stomach ache is a broad term for any abdominal pain or discomfort originating in the upper gastrointestinal tract. It can range from a dull ache after meals to sharp, cramping pains that wake you at night.
Weight loss refers to a reduction in total body mass, typically measured as a decrease in body weight on a scale. When it occurs unintentionally, it often signals an underlying medical issue.
Why a Painful Tummy Can Shrink Your Waistline
When your gut is irritated, the brain receives signals that alter two fundamental drivers of weight: calorie intake and metabolic rate. Here’s the chain reaction in plain English:
- Appetite suppression: Painful stretching of the stomach wall triggers the vagus nerve to send a “full” message to the brain, even if the stomach is empty. You feel less hungry and skip meals.
- Stress hormone surge: Chronic discomfort raises cortisol levels. While cortisol can promote fat storage, prolonged high levels also cause muscle breakdown (catabolism) and increase energy expenditure.
- Reduced nutrient absorption: Inflammation in the lining of the intestines (as seen in gastritis or inflammatory bowel disease) shortens the time food spends in the gut, so fewer nutrients make it into the bloodstream.
- Altered gut motility: Pain can speed up or slow down intestinal transit, leading to diarrhea or constipation, both of which can affect weight.
Put together, these mechanisms can shave off a few pounds each week without you even trying.
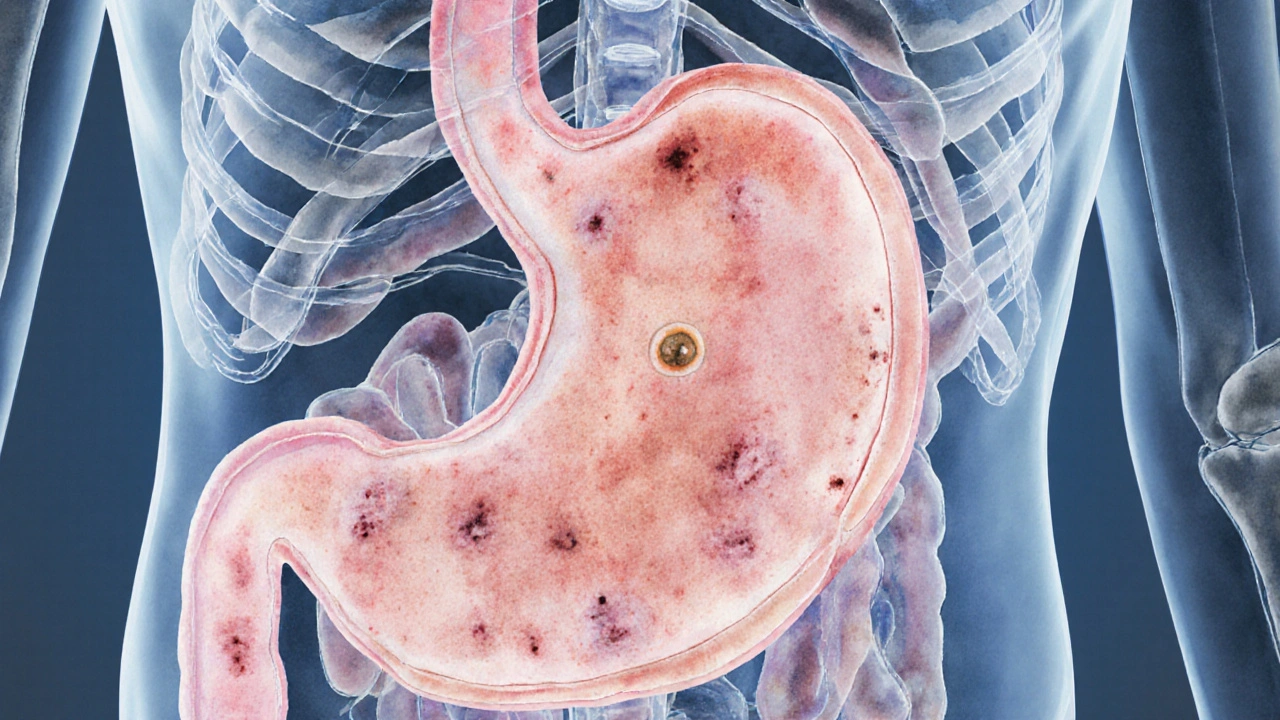
Common Conditions Where Stomach Ache Triggers Weight Loss
Not every tummy ache is created equal. Below is a snapshot of the most frequent diagnoses that pair pain with unintentional weight loss.
| Condition | Typical Pain Pattern | Why Weight Drops |
|---|---|---|
| Gastritis | Burning or gnawing after meals | Inflammation reduces appetite; acid damage impairs digestion. |
| Peptic ulcer | Sharp, nocturnal pain that eases with food | Fear of eating leads to chronic under‑eating. |
| Irritable bowel syndrome (IBS) | Cramping, bloating, alternating diarrhea/constipation | Irregular transit and stress‑related appetite loss. |
| Inflammatory bowel disease (IBD) | Persistent pain, blood in stool, urgency | Malabsorption and chronic inflammation burn calories. |
| Helicobacter pylori infection | Gnawing pain, especially when stomach is empty | Reduced food intake and ulcer formation. |
| Pancreatitis | Upper abdominal pain radiating to back | Enzyme deficiency hampers fat digestion; pain curbs eating. |
Notice a pattern? Most of these disorders either make eating uncomfortable or sabotage how your gut processes food.
When Weight Loss Is a Red Flag
Not every pound lost is a problem, but a rapid, unintentional drop-especially>5% of body weight in a month-should set off alarm bells. Here are three scenarios where the weight loss is more than a side‑effect.
- Gastrointestinal cancers: Tumors can cause obstruction, bleeding or severe inflammation, all of which lead to pain and cachexia (muscle wasting).
- Severe malabsorption syndromes such as celiac disease: The small intestine’s villi are damaged, so calories slip through the cracks.
- Systemic infections like tuberculosis or HIV: Chronic fever and cytokine release raise basal metabolic rate, burning calories even at rest.
If you’re experiencing any of the following alongside weight loss, book an appointment ASAP:
- Night sweats or persistent fever
- Blood in vomit or stool
- Unexplained fatigue despite adequate sleep
- Persistent vomiting or inability to keep food down
Practical Steps to Stop the Cycle
Below is a checklist you can start using tonight. It blends dietary tweaks, lifestyle habits and when to seek medical help.
- Track symptoms: Use a simple notebook or phone app to log pain intensity, timing, foods eaten, and weight changes. Patterns often reveal trigger foods.
- Adopt a gut‑friendly diet:
- Eat small, frequent meals (5‑6 per day) to avoid over‑stretching a tender stomach.
- Choose low‑fat, low‑spice options. Plain oatmeal, boiled potatoes, steamed carrots and lean protein (chicken breast, tofu) are easy on the lining.
- Include probiotic‑rich foods-yogurt, kefir, sauerkraut-to help rebalance gut bacteria.
- Stay hydrated: Sipping warm herbal teas (ginger or chamomile) can soothe the stomach and keep calories flowing.
- Manage stress: Practise deep‑breathing, 10‑minute meditation or a short walk after meals. Stress reduction lowers cortisol, which can otherwise exacerbate both pain and catabolism.
- Limit irritants: Alcohol, caffeine, nicotine and NSAIDs (ibuprofen, aspirin) are common culprits for gastritis and ulcers.
- Consider over‑the‑counter aids only after consulting a pharmacist or doctor. Antacids or H2 blockers can provide temporary relief while you investigate the cause.
- Schedule a check‑up if pain persists beyond two weeks, or if you lose more than 2kg (4.4lb) without trying.
Most people see improvement within a few weeks of these changes, especially when they address the underlying condition with proper medication.
What Your Doctor Might Do
If you end up seeing a clinician, expect a systematic approach:
- Medical history - Detailed interview about pain pattern, diet, stress, medication use.
- Physical exam - Palpation of abdomen, checking for tenderness or masses.
- Laboratory tests - CBC, ESR/CRP for inflammation, H. pylori breath test, stool studies for parasites.
- Imaging - Ultrasound or CT scan if obstruction or tumor suspected.
- Endoscopy - Direct visualisation of the stomach lining, useful for diagnosing ulcers or early cancer.
Based on findings, treatment may involve antibiotics (for H. pylori), proton‑pump inhibitors, steroids (for IBD), or surgery in severe cases.
Bottom Line
Stomach ache and weight loss are often two sides of the same coin. Pain reduces appetite, spikes stress hormones, and can impair nutrient absorption, all of which push the scale down. While many cases stem from relatively benign conditions like gastritis or IBS, a rapid, unexplained drop in weight should never be ignored. By logging symptoms, tweaking diet, managing stress, and seeking timely medical advice, you can break the cycle and keep both your gut and your weight in balance.

Frequently Asked Questions
Can occasional stomach pain cause weight loss?
A single episode usually doesn’t affect weight. The link appears when pain persists for weeks, because chronic discomfort consistently suppresses appetite and can interfere with digestion.
Should I stop eating when my stomach hurts?
Don’t skip meals completely. Instead, opt for bland, small portions that are easier on the stomach. Going too long without food can worsen irritation and trigger more stress hormones.
What foods are safest for a sensitive stomach?
Plain oatmeal, rice, boiled potatoes, steamed carrots, skinless chicken, and low‑fat yogurt are good choices. Avoid spicy sauces, fried foods, citrus, and caffeinated drinks until symptoms improve.
When is weight loss considered a medical emergency?
If you lose more than 5% of your body weight in a month, develop fever, notice blood in vomit or stool, or feel extreme weakness, seek medical attention right away.
Can stress alone cause both stomach pain and weight loss?
Yes. Stress releases cortisol, which can irritate the gut and suppress appetite. Over time, this can lead to chronic abdominal pain and gradual weight loss.

dAISY foto
September 29, 2025 AT 20:53Whoa, the gut‑brain highway is a wild roller‑coaster, and when the stomach throws a tantrum it messes with every scale we own.
Think about it: our bodies are tuned to protect us, so pain sends a frantic alarm that says “stop eating, something’s wrong!”
This forced fasting slashes calories before we even realize it.
Then there’s cortisol, that sneaky stress hormone, rising like a storm whenever discomfort lingers.
High cortisol not only torments our mood, it also hijacks muscle tissue for fuel, shaving off pounds you didn’t plan to lose.
Inflammation in the gut lining turns the nutrient‑rich buffet into a leaky sieve, letting vitamins slip through the cracks.
Not to forget gut motility – pain can speed things up into diarrhea or jam them into constipation, both of which can tip the scales.
The cascade repeats day after day, and before you know it, the number on the scale dwindles while you’re still battling that gnawing ache.
But fear not, brave reader, because understanding the mechanism is the first step to breaking the cycle.
Start logging your pain severity from 1 to 10, note the meals you skip, and watch the pattern emerge.
Swap heavy, greasy plates for bland, easy‑to‑digest meals – think oatmeal, boiled potatoes, and steamed carrots.
Small, frequent meals keep the stomach from over‑stretching and calm the vagus‑nerve “full” signal.
Hydration with warm ginger tea can soothe irritation while keeping calories flowing.
Stress‑relief practices – a short walk after eating, deep breathing, or a quick meditation – will tame cortisol spikes.
If the pain persists beyond two weeks or you’re shedding more than five percent of your weight, it’s time to see a doctor, because hidden ulcers, infections, or even early‑stage cancers love to hide behind vague discomfort.
Remember, the body is a brilliant teacher; listen to its warnings, feed it kindness, and the scale will settle into its rightful place.
David Stout
September 30, 2025 AT 16:20Hey folks, if your stomach’s acting up and the scale is sliding, you’re not alone – many of us have been there.
First thing is to keep a simple log of what you eat, how sore you feel, and any weight changes; patterns pop up fast.
Next, try soothing the gut with bland foods like bananas, rice, applesauce, and toast – the classic BRAT approach works wonders.
Stay hydrated, limit caffeine and alcohol, and give yourself permission to eat small meals more often.
And if the drop continues or pain worsens, don’t wait – schedule a check‑up; catching the root cause early makes recovery smoother.
Pooja Arya
October 1, 2025 AT 11:46Honestly, treating chronic stomach pain like a trivial inconvenience is a disservice to the body’s sacred signal system.
Our organs communicate distress; ignoring them is akin to walking past a fire alarm shouting “it’s fine.”
When you reduce intake merely to fit a fleeting aesthetic, you betray the very essence of self‑care.
Each pang is a moral compass pointing toward deeper imbalance – be it dietary, emotional, or pathological.
Embrace the discomfort as a teacher, not an enemy, and let it guide you toward genuine healing.
Only then will the weight loss cease being a silent confession of neglect.
Sam Franza
October 2, 2025 AT 07:13I agree, keep monitoring.
Raja Asif
October 3, 2025 AT 02:40Monitoring is fine but you also need to cut out the junk foods that America’s fast‑food empire pushes onto us; those processed meals are the real villains behind the pain and unwanted weight loss.
Matthew Tedder
October 3, 2025 AT 22:06Hey everyone, I totally get how unsettling it can feel watching the numbers drop while your stomach protests.
One thing that helped me was setting a gentle reminder to drink a glass of warm water with a pinch of salt every morning – it calms the gut and provides a tiny electrolyte boost.
Also, try journaling not just food, but moods and stressors; often the emotional spikes line up with the worst aches.
If you notice that pattern, a short mindfulness break before meals can make a big difference.
Remember, you’re not fighting this alone – community support and small consistent steps can bring the balance back.
Cynthia Sanford
October 4, 2025 AT 17:33Yaaas, those tiny habits are game‑changers! 🌟 I always keep a stash of ginger chews in my bag – when the cramp hits, a bite calms it fast and keeps my energy up so I dont lose any extra pounds.
Yassin Hammachi
October 5, 2025 AT 13:00Folks, let’s take a step back and view this from a systems perspective.
The stomach, brain, and endocrine axis form a feedback loop; when pain spikes, the hypothalamus tweaks hunger hormones like ghrelin and leptin.
This biochemical shift can suppress appetite even if you’re technically capable of eating.
Understanding this loop helps us target interventions – for instance, probiotic supplementation can modulate gut‑brain signaling and reduce both pain and appetite loss.
Couple that with low‑glycemic carbs to stabilize blood sugar, and you’ll see the weight stabilize without drastic dieting.
Michael Wall
October 6, 2025 AT 08:26In plain terms, ignoring the gut’s messages is like refusing to listen to a warning siren – you’ll end up paying a higher price later.
Irene Harty
October 7, 2025 AT 03:53It is worth contemplating that the pharmaceutical industry may have a vested interest in downplaying the correlation between chronic abdominal discomfort and involuntary weight loss, as it diverts attention from underlying lifestyle and environmental toxins that are more directly responsible for these symptoms.
Jason Lancer
October 7, 2025 AT 23:20Sure, but unless you have concrete evidence, it’s just a wild speculation that diverts resources from real medical research that could help patients in the meantime.
Brooks Gregoria
October 8, 2025 AT 18:46While most discussions praise the calculator as a handy tool, I’d argue that reducing a complex physiological process to a simple number risks oversimplifying patient experiences and may give a false sense of control.
Sumit(Sirin) Vadaviya
October 9, 2025 AT 14:13Indeed, the model is an approximation; nevertheless, it can serve as an educational aid to illustrate how pain severity and appetite reduction might interact. 😊 It’s not a diagnostic, but it encourages patients to track variables that are otherwise overlooked.
Theo Roussel
October 10, 2025 AT 09:40From a pathophysiological standpoint, the interplay between nociceptive signalling and hypothalamic appetite regulation involves intricate neuroendocrine cascades, including corticotropin‑releasing factor (CRF) and neuropeptide Y (NPY), which collectively modulate caloric intake and basal metabolic rate.
Erick Masese
October 11, 2025 AT 05:06Well put – in layman’s terms, the gut pain essentially tells the brain to “hold off on eating,” and the stress hormones then burn extra calories, leading to the weight dip you’re observing.
Matthew Charlton
October 12, 2025 AT 00:33Friends, if you’re feeling the weight slip away, consider adding a gentle, probiotic‑rich yogurt to your breakfast; the live cultures can help rebuild the intestinal lining and improve nutrient absorption.
Pair it with a modest portion of oatmeal for steady energy.
Consistency over perfection is key – small, sustainable changes win the battle.
Pamela may
October 12, 2025 AT 20:00Honestly, I think many people overlook how simple tweaks like the ones you mentioned can have monumental impacts on both gut health and overall metabolism; it’s not just about popping a probiotic or eating oatmeal, it’s about establishing a rhythm that your gastrointestinal system can adapt to, which in turn reduces inflammation, stabilizes the vagus nerve signalling, and ultimately curbs the involuntary weight loss that many experience when their stomach is constantly in a state of distress; moreover, incorporating daily mindfulness practices, even just five minutes of focused breathing after meals, can further modulate cortisol levels, creating a virtuous cycle of healing that reinforces the dietary adjustments you’re already making.
tierra hopkins
October 13, 2025 AT 15:26Keep at it, and remember that every mindful bite and gentle habit you add is a step toward bringing your weight back to a healthy, happy place.