Statin‑Antifungal Interaction: Rhabdomyolysis Risk Explained
 Oct, 26 2025
Oct, 26 2025
Statin-Antifungal Interaction Risk Calculator
Risk Assessment Tool
Enter specific statin and azole combination details to determine risk level and clinical recommendations.
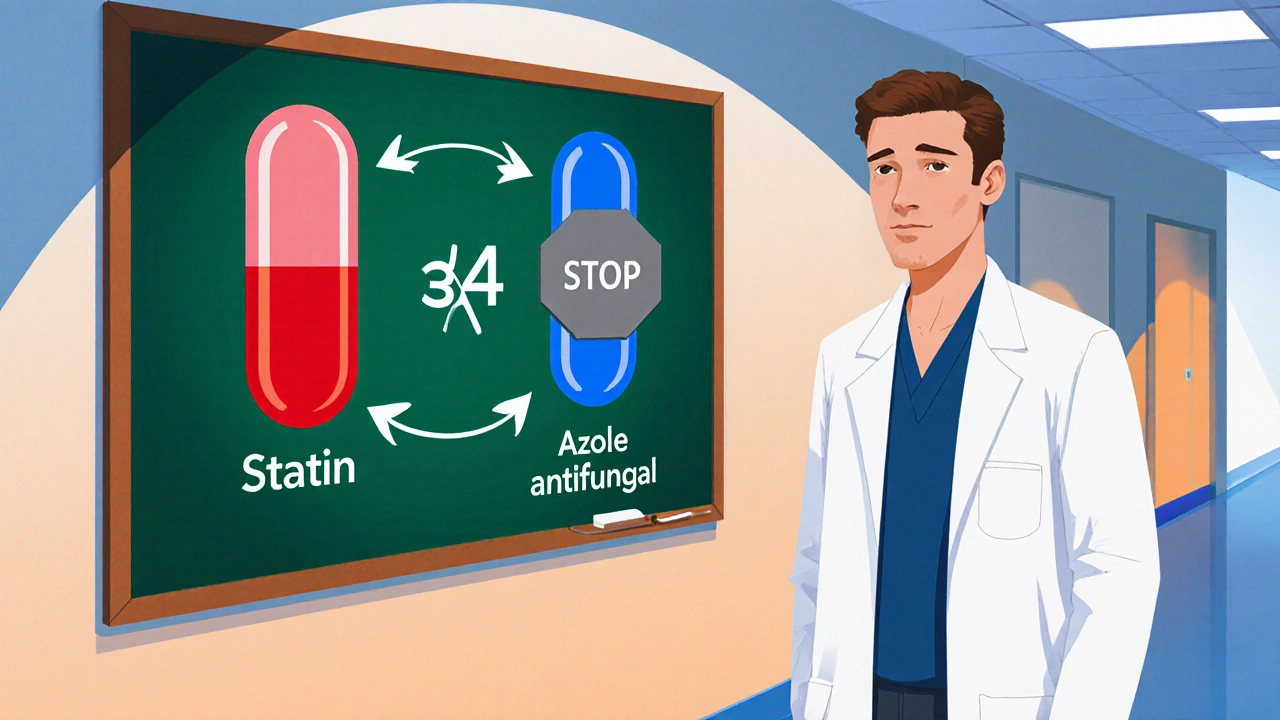
When patients take Statins HMG‑CoA reductase inhibitors that lower cholesterol and reduce cardiovascular events together with an Azole antifungal medication a class of drugs used to treat fungal infections such as candidiasis and aspergillosis, the chance of developing severe muscle damage jumps dramatically. This article walks you through why the combo is risky, how the body’s chemistry creates the problem, and what clinicians do to keep patients safe.
Why the Combination Matters
The heart of the issue is the liver enzyme CYP3A4. Many statins - specifically lovastatin, simvastatin, and atorvastatin - are cleared from the body primarily by this enzyme. Azole antifungals, especially ketoconazole, itraconazole, and voriconazole, are powerful inhibitors of CYP3A4. When the enzyme is blocked, statin levels can rise 5‑ to 20‑fold, pushing the drug into a toxic range.
One of the most feared outcomes is rhabdomyolysis, a condition where muscle fibers break down, release their contents into the bloodstream, and can cause kidney failure. In everyday statin use, rhabdomyolysis occurs in roughly 0.1‑0.5 per 10,000 person‑years. When a strong CYP3A4 inhibitor is added, the risk spikes 10‑ to 20‑fold, according to multiple clinical studies.
Metabolic Pathways: Who Gets Metabolized By CYP3A4?
Not all statins behave the same way. Here’s a quick snapshot:
- High CYP3A4 dependence: lovastatin, simvastatin, atorvastatin
- Low or negligible CYP3A4 dependence: pravastatin, rosuvastatin, fluvastatin
Similarly, azoles differ in how strongly they inhibit CYP3A4:
- Ketoconazole - Ki 0.004‑0.02 µM (very strong)
- Itraconazole - Ki 0.1‑0.5 µM (strong)
- Voriconazole - Ki 0.5‑1.0 µM (moderate‑strong)
- Fluconazole - Ki 5‑10 µM (moderate, dose‑dependent)
Because of these differences, clinicians can predict which pairings are most hazardous.
High‑Risk Pairings: Numbers That Matter
A 2017 clinical pharmacology study showed the following area‑under‑the‑curve (AUC) increases when simvastatin is taken with itraconazole:
- Simvastatin AUC ↑ 1,160 % (more than ten‑fold)
- Lovastatin AUC ↑ 1,550 %
- Atorvastatin AUC ↑ 360 %
Fluconazole, even at a high 400 mg/day dose, still raises simvastatin AUC by about 350 % and atorvastatin by 80 %.
Real‑world data from the FDA Adverse Event Reporting System (FAERS) recorded 1,247 rhabdomyolysis cases linked to statin‑azole combos from 2010‑2019. Simvastatin‑itraconazole alone accounted for 38.7 % of those reports.
| Statin | Azole | Relative Risk ↑ | FDA Recommendation |
|---|---|---|---|
| Simvastatin (≥20 mg) | Itraconazole / Ketoconazole | 22‑fold | Contraindicated |
| Simvastatin (≤10 mg) | Fluconazole | 3‑4‑fold | Maximum 10 mg daily |
| Atorvastatin (≤20 mg) | Fluconazole | 1.8‑fold | Limit to 20 mg |
| Pravastatin | Any azole | ≈1‑fold | No dose change needed |
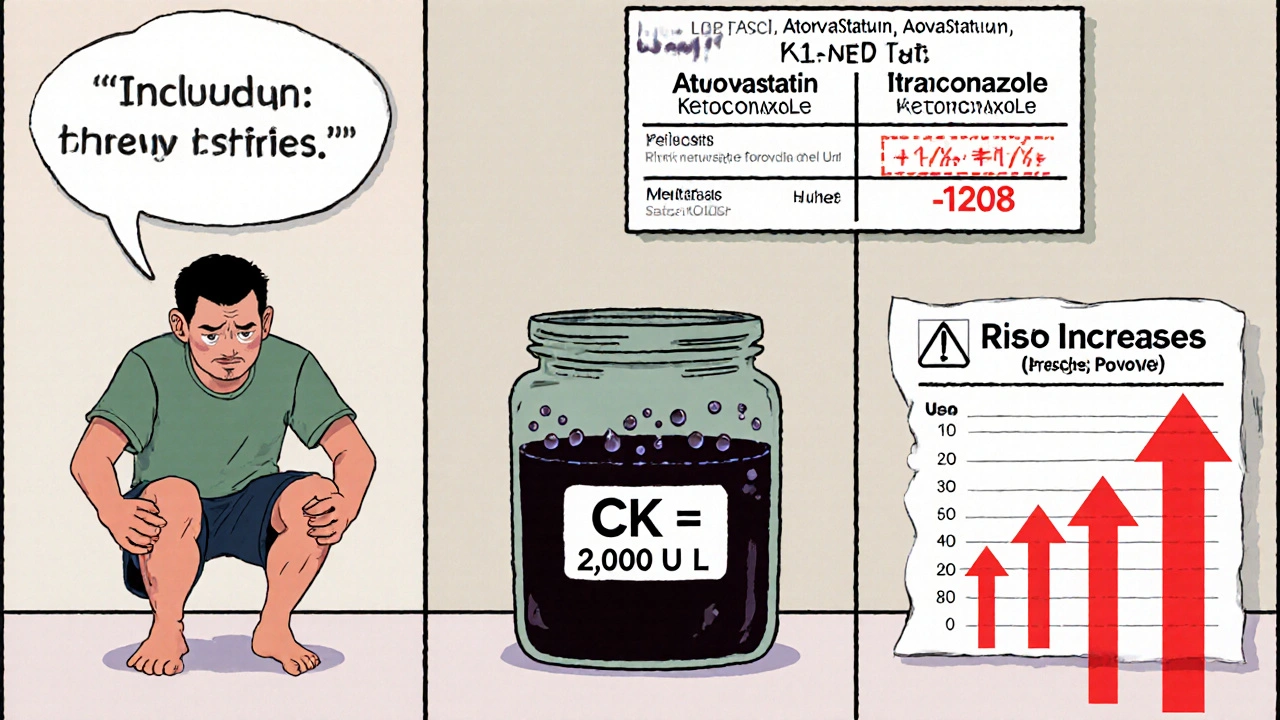
Clinical Signs: What to Watch For
Patients typically notice problems within the first 1‑2 weeks of starting the antifungal. The most common symptoms are:
- Severe muscle pain or weakness (reported in 92 % of cases)
- Dark‑colored urine (76 %)
- Generalized fatigue or cramps (88 %)
Laboratory confirmation comes from a creatine kinase (CK) test. Levels above 10 times the upper limit of normal (often >2,000 U/L) signal impending rhabdomyolysis and demand immediate statin discontinuation.
Case reports illustrate the severity. A 68‑year‑old male on simvastatin 40 mg plus fluconazole 200 mg for onychomycosis developed CK = 18,400 U/L after just seven days, requiring three days of hospitalization.
Management Strategies: How Clinicians Reduce the Risk
Guidelines published in 2023 outline a step‑by‑step approach:
- Assess need for both drugs. If the antifungal is short‑term, consider pausing the statin or switching to a low‑risk statin.
- Choose a safer statin. Pravastatin (40 mg), fluvastatin (80 mg), or rosuvastatin (≤20 mg) are minimally affected by azoles.
- Adjust dose. For moderate inhibitors like fluconazole, limit simvastatin to 10 mg daily and atorvastatin to 20 mg.
- Monitor CK. Obtain a baseline CK before starting the combo, then repeat weekly. Stop the statin if CK > 10× ULN or if severe symptoms appear.
- Resume safely. After finishing the azole, wait 2‑3 days (or the drug’s half‑life) before restarting the original statin dose.
Electronic health record (EHR) systems have helped. A 2022 Mayo Clinic study showed that hard stops for simvastatin > 20 mg plus itraconazole cut contraindicated orders by 87 %.
Alternative Antifungals: When You Need Something Safer
Isavuconazole, approved in 2015, has a Ki > 20 µM for CYP3A4 - essentially negligible inhibition. Clinical trials found no significant change in simvastatin levels when the two were co‑administered, making it a preferred option for patients who cannot switch statins.
Another emerging class, tetrazoles, is still in phase II trials but shows promise for a low interaction profile.

Checklist for Prescribers
- Identify statin type and dose.
- Determine azole potency (strong, moderate, weak).
- Consult the risk table - avoid contraindicated combos.
- If combination unavoidable, switch to pravastatin, fluvastatin, or rosuvastatin.
- Order baseline CK; repeat weekly.
- Educate patient on muscle pain warning signs.
- Document decision and monitoring plan in the EHR.
Future Directions: Pharmacogenomics and Decision Support
Research in 2022 linked the CYP3A5*3/*3 genotype to a 2.3‑fold increase in statin toxicity during azole therapy. As genotyping becomes routine, clinicians may soon get automated alerts that factor in a patient’s metabolic genotype.
The American College of Cardiology and Infectious Diseases Society of America are co‑authoring joint guidelines slated for 2024. These will likely feature algorithms that incorporate age, renal function, genotype, and drug‑specific interaction strength, moving beyond the one‑size‑fits‑all tables we use today.
Bottom Line
When you pair statins with azole antifungals, you’re playing with a biochemical shortcut that can turn a routine cholesterol pill into a life‑threatening muscle toxin. Understanding which statins are CYP3A4‑dependent, recognizing the potency of each azole, and following a monitoring protocol can prevent most severe outcomes. Switch to a low‑risk statin or a non‑CYP3A4‑inhibiting antifungal whenever possible, keep an eye on CK, and leverage EHR alerts. With those steps, the benefits of both drugs stay intact while the danger of rhabdomyolysis stays far away.
Which statins are safest to use with azole antifungals?
Pravastatin, fluvastatin, and rosuvastatin have little to no CYP3A4 metabolism, so they remain largely unaffected by azoles. They are the preferred choices when an antifungal is needed.
What CK level should trigger immediate statin discontinuation?
A CK value greater than ten times the upper limit of normal (usually >2,000 U/L) or a rapid rise accompanied by muscle pain warrants stopping the statin right away.
Can fluconazole be used safely with simvastatin?
Fluconazole is a moderate CYP3A4 inhibitor. If simvastatin must be continued, the dose should be limited to 10 mg daily, and CK monitoring is essential.
What alternative antifungal has minimal interaction with statins?
Isavuconazole shows very weak CYP3A4 inhibition and has not demonstrated clinically relevant statin interactions, making it a safer option for patients on high‑risk statins.
How often should CK be checked during combined therapy?
Baseline CK before starting the combo, then weekly checks for the first two weeks. Continue bi‑weekly if the patient remains symptom‑free.

Erik Redli
October 26, 2025 AT 13:00Look, the hype around statin‑azole interactions is just another fear‑mongering campaign. Doctors love to throw around “rhabdomyolysis” like it’s a death sentence, but the real data shows it’s a rarity even when you mix the drugs. Most patients on simvastatin and fluconazole never develop CK spikes; you’d need a genetic defect or severe renal failure for that to happen. The CYP3A4 inhibition numbers are impressive on paper, but in real‑world practice the body compensates with alternate pathways. If you’re worried, just drop the statin for a week and you’ll be fine – you won’t magically develop heart disease overnight. The FDA warnings are more about legal liability than patient safety. Remember, pharma pushes the narrative to keep you on brand‑name meds and sell more expensive alternatives like ezetimibe. A low‑dose pravastatin is cheap, but why bother when you can just monitor CK once a month? In short, don’t let a fancy enzyme name dictate your prescribing; use clinical judgment, not scare tactics. Stay skeptical, stay calm, and keep the prescription pad moving.
Statins have been proven to reduce mortality, and a brief interruption won’t erase years of benefit. If you do need an azole, consider therapeutic drug monitoring instead of blanket discontinuation. Switching to rosuvastatin just because of a label is overkill and wastes time. Patients appreciate clear instructions, not endless warnings that make them anxious. Bottom line: balance risk with benefit, not fear.
Monika Pardon
October 26, 2025 AT 14:23Ah yes, the classic “big pharma” plot where they hide the fact that azoles are actually a front for mind‑control nanobots. Obviously the CYP3A4 inhibition data is fabricated to keep us dependent on their patented statins. If you read the fine print, you’ll see that every “clinical study” is funded by the cholesterol‑pill lobby. The truth is they want you to believe a simple drug‑drug interaction will kill you, so you’ll buy the newer, pricier alternatives they push. Of course, the government agencies are in on it, too – they love to publish risk tables that look scientific but are really just marketing fluff. So, when a paper tells you to avoid simvastatin with itraconazole, just remember who benefits from that advice. In reality, most people take a supplement, a fungal infection, and live happily, never hearing about rhabdo. The whole thing feels like a staged drama designed to keep the “watch‑and‑wait” narrative alive. Nonetheless, if you must prescribe, you could sprinkle a disclaimer that the “real risk” is probably the hidden micro‑chips.
Dave Sykes
October 26, 2025 AT 15:46Team, when you have a patient who needs both a statin and an azole, the first move is to evaluate the necessity of each. Pull the medication list, check the statin’s CYP3A4 dependence, and ask yourself if the antifungal can be swapped for a non‑inhibitor. If the statin is high‑risk like simvastatin ≥20 mg, either pause it or switch to pravastatin, fluvastatin, or rosuvastatin before starting the azole. Set a baseline CK, then schedule weekly checks for the first two weeks – that’s where you’ll catch any early spikes. Communicate the warning signs clearly: sudden muscle pain, dark urine, or unexplained fatigue. Should CK climb above ten times the upper limit, stop the statin immediately and reassess the antifungal regimen. Document every decision in the EHR; a hard stop alert can save you from an accidental contraindicated order. Remember, the goal is to treat the infection while protecting the muscle, not to abandon either therapy. Keep the plan simple, monitor closely, and adjust doses as needed – that’s the winning strategy.
Erin Leach
October 26, 2025 AT 17:10I hear how stressful it can be when you’re juggling a cholesterol pill and a fungal infection at the same time. The fear of muscle damage is real, especially after reading about rhabdomyolysis cases. It helps to know that not every combination leads to trouble – low‑risk statins like pravastatin are usually fine. Keeping an eye on CK levels for the first couple of weeks can give you peace of mind and catch any problems early. If you notice any unusual soreness or dark urine, reach out to your doctor right away; they can adjust the therapy before anything serious develops. Remember, you’re not alone in this – many patients navigate these meds successfully with the right monitoring. Stay proactive, ask for clear instructions, and trust that the care team is looking out for you.
Carla Smalls
October 26, 2025 AT 18:33Great point to remember that there are safer statin options when an azole is unavoidable. Choosing pravastatin or rosuvastatin can keep the interaction risk low while still providing cardiovascular protection. A small dose adjustment of the azole, like using fluconazole instead of itraconazole, also reduces the CYP3A4 inhibition. Pairing these strategies with routine CK checks creates a solid safety net. Patients often feel reassured when they see a clear plan that balances infection control with heart health. Keep sharing these practical tips – they make a real difference in everyday practice.
Jennyfer Collin
October 26, 2025 AT 19:56It is quite evident that the “official” risk tables are a convenient way for the pharmaceutical conglomerates to steer prescribing habits toward their high‑margin products 🧐. By insisting on switching to generic pravastatin, they are effectively pushing clinicians into a niche market where they can sell monitoring kits at premium prices 📈. The subtle inclusion of “monitor CK weekly” feels like a hidden directive to keep patients in constant contact with the healthcare system, generating additional billing opportunities. Of course, the agencies will argue it’s patient safety, but one must wonder whose safety is truly prioritized. In any case, a pragmatic approach-using non‑CYP3A4 inhibitors like isavuconazole and low‑interaction statins-sidesteps the manufactured scarcity they seem to be creating. 🤓
Jay Campbell
October 26, 2025 AT 21:20Monitoring CK is essential.
Laura Hibbard
October 26, 2025 AT 22:43Sure, let’s all panic and ban every statin‑azole combo because a handful of case reports exist, while ignoring that millions tolerate these meds daily without a hitch. The real solution is a balanced protocol: assess necessity, pick a low‑risk statin, set a baseline CK, and keep an eye on symptoms. That way we avoid needless alarmism and still protect patients from genuine harm. It’s a win‑win, not a headline‑grabbing drama.