Severe Pancreatitis from Medications: Warning Signs and Treatment
 Nov, 14 2025
Nov, 14 2025
What Is Drug-Induced Severe Pancreatitis?
Drug-induced severe pancreatitis is when a medication triggers dangerous inflammation of the pancreas - a gland behind your stomach that helps digest food and regulate blood sugar. Unlike pancreatitis caused by gallstones or alcohol, this form happens because a drug directly harms the pancreas. It’s rare - only about 1.4% to 3.6% of all acute pancreatitis cases come from medications - but when it happens, it can turn life-threatening fast. About 20% of these drug-related cases are severe, with mortality rates between 15% and 30%. The good news? If caught early and the drug is stopped, many people recover fully.
Who’s at Risk?
Anyone taking certain medications can develop this, but some groups are more vulnerable. People over 60 are at highest risk, mostly because they’re on more medications - an average of 5.2 per person compared to 2.7 in younger adults. Those with chronic conditions like Crohn’s disease, diabetes, or high blood pressure are also more likely to be on high-risk drugs. If you’re taking more than three prescriptions, especially long-term, your risk goes up. It’s not always obvious who will react. Some people develop symptoms after just a few days. Others take the same drug for years before something flips.
Which Medications Are Most Likely to Cause It?
Eight drug classes have strong evidence linking them to severe pancreatitis. These aren’t obscure drugs - many are prescribed daily.
- ACE inhibitors like lisinopril and enalapril - used for high blood pressure
- Diuretics like furosemide and hydrochlorothiazide - water pills
- Statins like simvastatin and atorvastatin - cholesterol-lowering drugs
- Antidiabetic drugs including exenatide (Byetta) and sitagliptin (Januvia)
- Valproic acid - used for seizures and bipolar disorder
- Azathioprine - an immunosuppressant for autoimmune diseases
- Oral contraceptives with ethinyl estradiol
- SGLT2 inhibitors like canagliflozin and dapagliflozin - newer diabetes drugs
Valproic acid and azathioprine are especially dangerous. Studies show 22% of people on valproic acid develop necrotizing pancreatitis - where parts of the pancreas die. For azathioprine, it’s 18%. These aren’t rare side effects - they’re serious enough that the FDA and EMA have added black box warnings.
Warning Signs You Can’t Ignore
The pain is the biggest red flag. It usually starts as a deep, constant ache in the upper abdomen, just below the ribs. It doesn’t come and go - it stays. Within hours, it often radiates straight through to your back. Many people say it feels like a band tightening around their middle. You might also feel nauseous, vomit, or have a fever. Unlike gallstone pain, which hits suddenly after eating fatty food, drug-induced pain builds slowly - often over days or weeks after starting or increasing a medication.
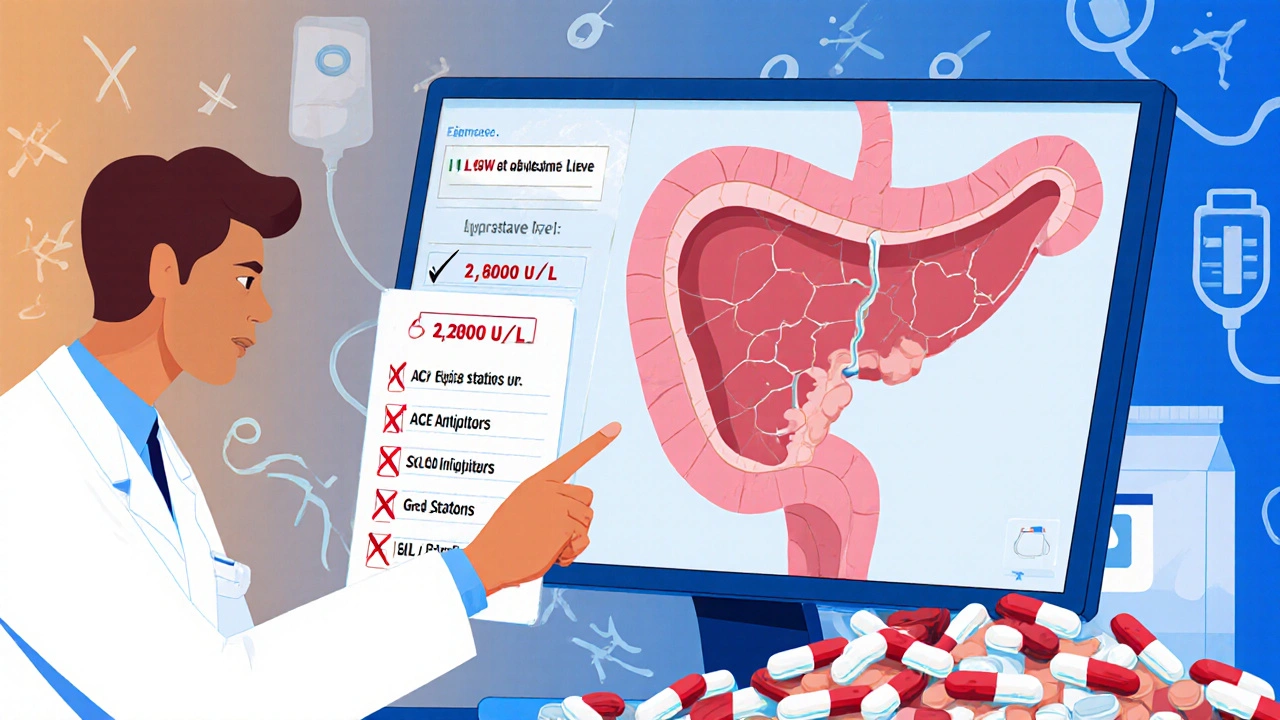
Other signs include rapid heartbeat, shallow breathing, or feeling dizzy. These mean your body is going into shock. If you’re on any of the high-risk drugs above and have this kind of pain, don’t wait. Don’t assume it’s heartburn or gas. Get your lipase levels checked. A level three times above normal confirms pancreatitis. A level over 1,000 U/L is common in severe cases - one patient reported 2,800 U/L after taking simvastatin for three years.
Why Diagnosis Is Often Delayed
Doctors miss this diagnosis all the time. Why? Because the symptoms look like other common problems - gastritis, gallbladder attacks, even heart issues. A patient on azathioprine for Crohn’s was told her pain was "just acid reflux" for weeks. By the time a CT scan was done, 40% of her pancreas was dead. She spent three weeks in the ICU. That’s not unusual. In fact, 68% of people with drug-induced pancreatitis say they were misdiagnosed at first. The delay costs lives. The longer you wait to stop the drug, the worse it gets.
How It’s Treated - Step by Step
There’s no magic pill. Treatment is about support and stopping the cause.
- Stop the drug immediately. This is non-negotiable. If you suspect your medication is the cause, stop taking it - but only after talking to your doctor. Never quit cold turkey without medical advice, especially for drugs like blood pressure or seizure meds.
- IV fluids. You’ll get 250-500 mL per hour of fluids through an IV. This keeps your pancreas from drying out and helps flush out toxins. Doctors monitor your hematocrit to keep it between 35% and 44% - too low means you’re not getting enough fluid; too high means you’re dehydrated.
- Pain control. Acetaminophen (Tylenol) is the first choice. If that’s not enough, low-dose morphine is used. Avoid ibuprofen or naproxen - they can make things worse.
- Feed your gut, not your stomach. You’ll be told not to eat or drink (NPO) at first. But within 24-48 hours, if you can’t eat, you’ll get nutrition through a tube placed past your stomach into your small intestine. This reduces complications and speeds recovery.
- Watch for infection. Antibiotics aren’t given unless the pancreas tissue dies and gets infected. Then, meropenem is the go-to drug.
Most people start feeling better in 3-5 days if the drug is stopped early. But if you wait more than 24 hours to stop the medication, your risk of complications jumps by 37%.
What Happens After Recovery?
If you survive the acute phase, you’ll need follow-up. Your doctor will likely order a repeat CT scan to check for scarring or fluid collections. Some people develop chronic pancreatitis later, especially if they had necrosis. You’ll also need to avoid all the drugs that caused the problem - and possibly others in the same class. For example, if lisinopril caused it, avoid all ACE inhibitors. If you had a statin-induced attack, you won’t be able to take any statin again. Some people switch to non-statin cholesterol drugs like ezetimibe or PCSK9 inhibitors.
How to Protect Yourself
If you’re on one of the high-risk medications, here’s what to do:
- Know the symptoms - abdominal pain that won’t quit, radiating to your back.
- Ask your doctor: "Could this drug cause pancreatitis?" Don’t be shy. Many don’t bring it up unless you do.
- Get a baseline lipase test before starting a new high-risk drug - especially if you’re over 60 or on multiple meds.
- Track your meds. Use a phone app or written list. Note when you started each drug and any new symptoms.
- If you develop unexplained abdominal pain while on one of these drugs, demand a lipase test. Don’t settle for "it’s probably just indigestion."
Why This Is Getting Worse
Drug-induced pancreatitis is rising. The FDA logged over 4,200 cases in 2022 - up 13% from the year before. Newer drugs, like SGLT2 inhibitors for diabetes, are now being linked to more cases. In 2023, the FDA added stronger warnings for these drugs after 87 cases in just 18 months. At the same time, more older adults are on multiple prescriptions. By 2035, experts predict a 25% increase in these cases. Hospitals are starting to use electronic alerts in their systems to flag high-risk combinations - but that’s still not universal. You can’t rely on the system to protect you. You have to be your own advocate.
Real Stories - What Patients Are Saying
On patient forums, the same pattern keeps showing up. A 45-year-old woman on lisinopril for hypertension woke up at 3 a.m. with pain so bad she couldn’t breathe. Her lipase was 1,250. She spent five days in the hospital. After stopping the drug, she’s been fine for over a year. A 62-year-old man on simvastatin for three years had the same story - pain, high lipase, stopped the statin, improved in 72 hours. One Reddit post from a doctor said: "I’ve seen this three times now. Every time, the patient had been told it was "just a stomach bug." They all got better after stopping the drug. Why isn’t this taught in medical school?"
Final Thought
Drug-induced severe pancreatitis isn’t something you can ignore. It doesn’t always come with a warning label. It doesn’t always show up on blood tests right away. But it’s real, it’s dangerous, and it’s often reversible - if you act fast. If you’re on a high-risk medication and feel unusual, persistent pain in your upper belly, don’t wait. Don’t hope it goes away. Get checked. Your pancreas can’t wait.
Can you get pancreatitis from over-the-counter meds?
Yes. While most cases come from prescription drugs, some OTC meds have been linked. High doses of ibuprofen or naproxen over long periods can rarely trigger pancreatitis. Even some herbal supplements like green tea extract or kava have been reported in case studies. The risk is low, but if you’re taking multiple supplements or high-dose NSAIDs and develop abdominal pain, it’s worth mentioning to your doctor.
How long after starting a drug does pancreatitis usually appear?
It varies. For some drugs like ACE inhibitors or statins, symptoms can appear after just a few days. For others, like azathioprine or valproic acid, it might take weeks or months. On average, symptoms start 7 to 14 days after beginning the medication. But there are cases where people developed it after 2 years of use. There’s no safe timeline - any new pain while on a high-risk drug should be checked.
Can you ever take the drug again after recovering?
No. Once you’ve had drug-induced pancreatitis from a specific medication, you should never take it again - or any drug in the same class. Re-exposure almost always causes a recurrence, often more severe. Even if you feel fine months later, the risk is too high. Your doctor will find alternatives. For example, if you had pancreatitis from lisinopril, you’d switch to a calcium channel blocker like amlodipine instead.
Is there a blood test that confirms it’s drug-induced?
No single test can prove a drug caused it. Diagnosis relies on timing: symptoms appearing after starting the drug, no other clear cause (like gallstones or alcohol), and improvement after stopping it. If your lipase is high and you’re on a known offender, and other causes are ruled out, doctors classify it as "probable" drug-induced. A "definite" diagnosis would require re-challenging you with the drug - but that’s rarely done because it’s dangerous.
Can pancreatitis from medication cause permanent damage?
It can. If the inflammation is severe and lasts too long, parts of the pancreas can die (necrosis) and form scar tissue. This can lead to chronic pancreatitis, where you lose digestive enzyme production and may need lifelong enzyme supplements. You could also develop diabetes if insulin-producing cells are damaged. Early treatment and stopping the drug quickly greatly reduce this risk.
Are younger people at risk too?
Yes, but less commonly. Most cases are in people over 60 because of polypharmacy. But younger people on azathioprine for Crohn’s or lupus, or those on oral contraceptives, can develop it too. A 28-year-old woman on birth control pills developed severe pancreatitis after six months. Her case was rare, but it happened. Age doesn’t make you immune - the drug and your body’s reaction matter more.

Mqondisi Gumede
November 16, 2025 AT 04:06Douglas Fisher
November 17, 2025 AT 17:51Albert Guasch
November 19, 2025 AT 15:40Ginger Henderson
November 21, 2025 AT 14:13Bethany Buckley
November 22, 2025 AT 17:55Stephanie Deschenes
November 23, 2025 AT 09:05Cynthia Boen
November 24, 2025 AT 07:22Amanda Meyer
November 24, 2025 AT 21:21Jesús Vásquez pino
November 25, 2025 AT 11:36hannah mitchell
November 26, 2025 AT 21:36vikas kumar
November 27, 2025 AT 09:09Vanessa Carpenter
November 28, 2025 AT 01:16Bea Rose
November 29, 2025 AT 05:35Michael Collier
November 29, 2025 AT 20:15Shannon Amos
December 1, 2025 AT 09:27stephen riyo
December 2, 2025 AT 17:07