Pulmonary Function Tests: How to Interpret Spirometry and DLCO Results
 Nov, 20 2025
Nov, 20 2025
When your doctor orders a pulmonary function test, it’s not just another checkbox. It’s a window into how well your lungs are actually working-especially if you’re struggling with shortness of breath, chronic cough, or just don’t feel like yourself when you climb stairs. Two tests stand out as the backbone of lung evaluation: spirometry and DLCO. Together, they tell a story that neither can tell alone.
What Spirometry Really Measures
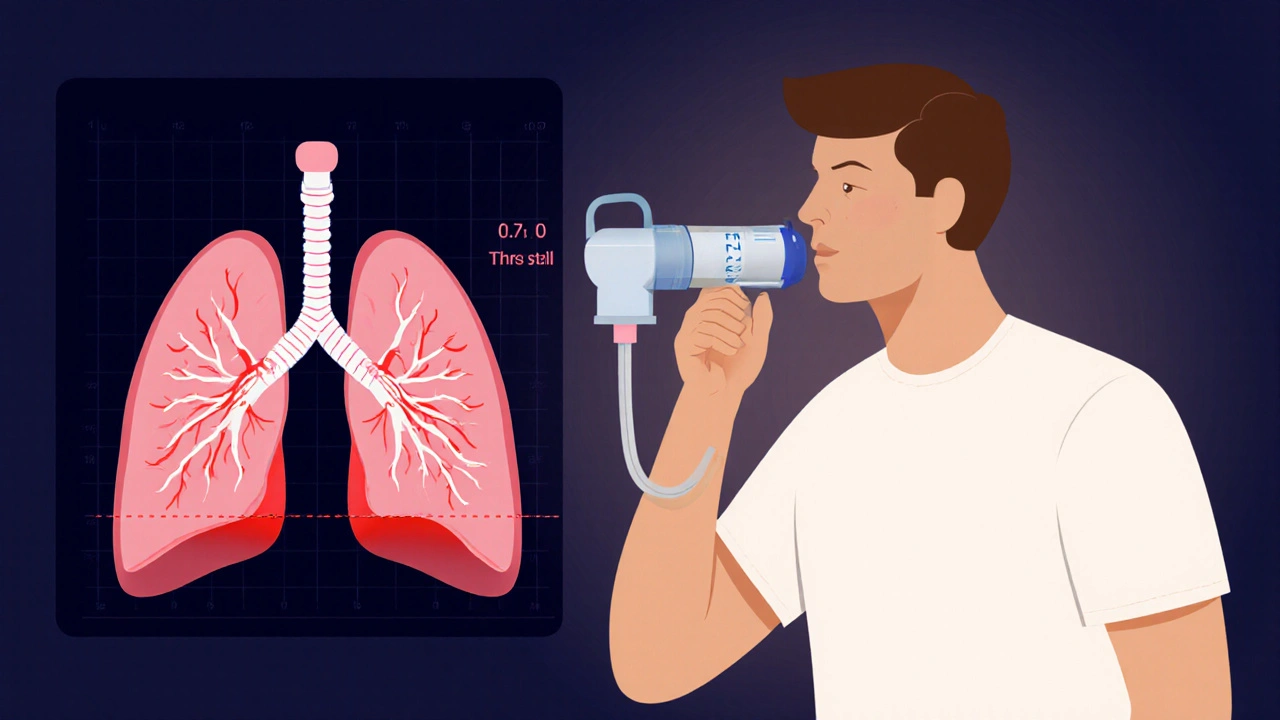
Spirometry is the most common lung test you’ll ever take. You breathe in as deeply as you can, then blow out as hard and fast as you can into a tube connected to a machine. That’s it. No needles, no radiation, no waiting. But what the machine records is anything but simple. It measures two key numbers: FEV1 (how much air you can force out in the first second) and FVC (how much air you can force out total). The ratio between them-FEV1/FVC-is the real clue. If that ratio drops below 0.7, you likely have airflow obstruction. That’s the hallmark of asthma, COPD, or chronic bronchitis. But here’s where people get confused: a low FVC doesn’t always mean your lungs are stiff. Sometimes, it’s because you’re trapped in your own air. In severe asthma or emphysema, you can’t fully empty your lungs, so your FVC looks low even though your lung tissue is normal. That’s called "pseudorestriction." Without more info, you might think you have scarring in your lungs when you don’t.What DLCO Adds That Spirometry Can’t
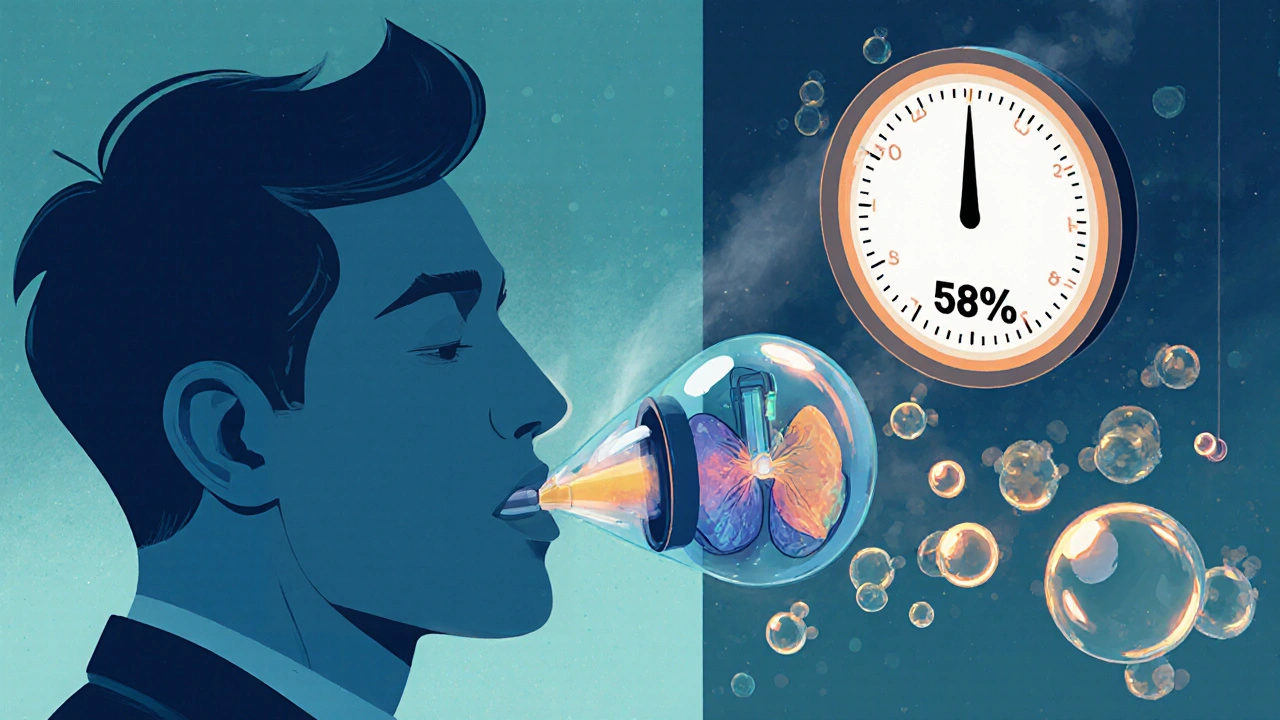
DLCO-diffusing capacity of the lung for carbon monoxide-is the less-known but far more revealing test. It doesn’t measure how much air you can move. It measures how well oxygen gets from your lungs into your blood. Here’s how it works: you inhale a tiny, harmless amount of carbon monoxide mixed with helium and oxygen. You hold your breath for exactly 10 seconds, then exhale. The machine compares how much CO you breathed in versus how much you breathed out. The difference tells you how efficiently your lungs transfer gas. Normal DLCO is between 75% and 140% of what’s predicted for your age, height, and sex. Below 75%? Something’s wrong with the air sacs or blood vessels. Above 140%? That’s unusual but can happen in asthma, polycythemia, or even bleeding in the lungs. The real power of DLCO shows up when spirometry looks normal but you still feel breathless. If your DLCO is low, your lungs are failing at gas exchange-even if airflow is fine. That’s a red flag for early interstitial lung disease, pulmonary hypertension, or even hidden pulmonary emboli. In fact, DLCO can drop by 30-40% before spirometry shows any change. That’s a 12- to 18-month head start on diagnosis.Putting It Together: Real Patterns, Real Diagnoses
You can’t interpret these tests in isolation. You need to look at both together. Here’s what the numbers mean in practice:- Low FEV1/FVC + Normal DLCO → Classic obstructive disease like asthma or COPD. The airways are narrowed, but gas exchange is still okay.
- Low FVC + Low DLCO → Restrictive disease with lung damage. Think pulmonary fibrosis, sarcoidosis, or asbestosis. The lungs are stiff and can’t transfer oxygen well.
- Low FVC + Normal DLCO → Restriction without lung damage. Could be obesity, scoliosis, or weak breathing muscles. Your lungs are physically restricted, but the tissue itself is healthy.
- Normal spirometry + Low DLCO → This is the sneaky one. You feel breathless, but your airflow is fine. Could be early interstitial lung disease, pulmonary hypertension, or even chronic blood clots in the lungs. This is where DLCO saves lives.
- High DLCO + Normal spirometry → Less common. Seen in asthma attacks, polycythemia (too many red blood cells), or pulmonary hemorrhage. Also common in smokers-because CO from cigarettes sticks to hemoglobin and tricks the test.
Why DLCO Is Often Misunderstood
Even among doctors, DLCO is the most misinterpreted test. Why? Because it’s sensitive to things you might not think about. - Hemoglobin levels: If you’re anemic, your DLCO drops. Every 1 g/dL drop in hemoglobin lowers DLCO by about 1%. If your hemoglobin wasn’t checked before the test, you might think you have lung disease when you just need iron. - Carbon monoxide from smoking: Even if you quit last week, CO in your blood can falsely lower your DLCO by 5-10%. That’s why you’re asked not to smoke for at least 24 hours before the test. - Breath-hold timing: If you hold your breath for 8 seconds instead of 10, your DLCO will read lower. If you exhale too fast, the machine can’t measure accurately. That’s why the test needs to be done by trained staff using standardized protocols. - Age and sex: DLCO naturally declines with age. Men have higher values than women. Reference values must be adjusted properly-otherwise, you’ll misdiagnose healthy older adults.When DLCO Changes Everything
I’ve seen patients come in with normal spirometry, no wheezing, no cough, but they’re too breathless to walk to the mailbox. Their DLCO is 58%. That’s not normal. That’s early lung scarring. In pulmonary fibrosis, DLCO is often the first and most sensitive marker. One patient I worked with had an FVC of 65% (mildly reduced) but a DLCO of 22%. That’s severe. Her survival odds dropped dramatically. That number guided her treatment-she started antifibrotic drugs early, before her lungs got worse. In pulmonary hypertension, the ratio of FVC to DLCO is more telling than either number alone. If it’s above 1.6, there’s a 92% chance you have high pressure in your lung arteries. That’s a game-changer. It means you need an echocardiogram, not just more inhalers.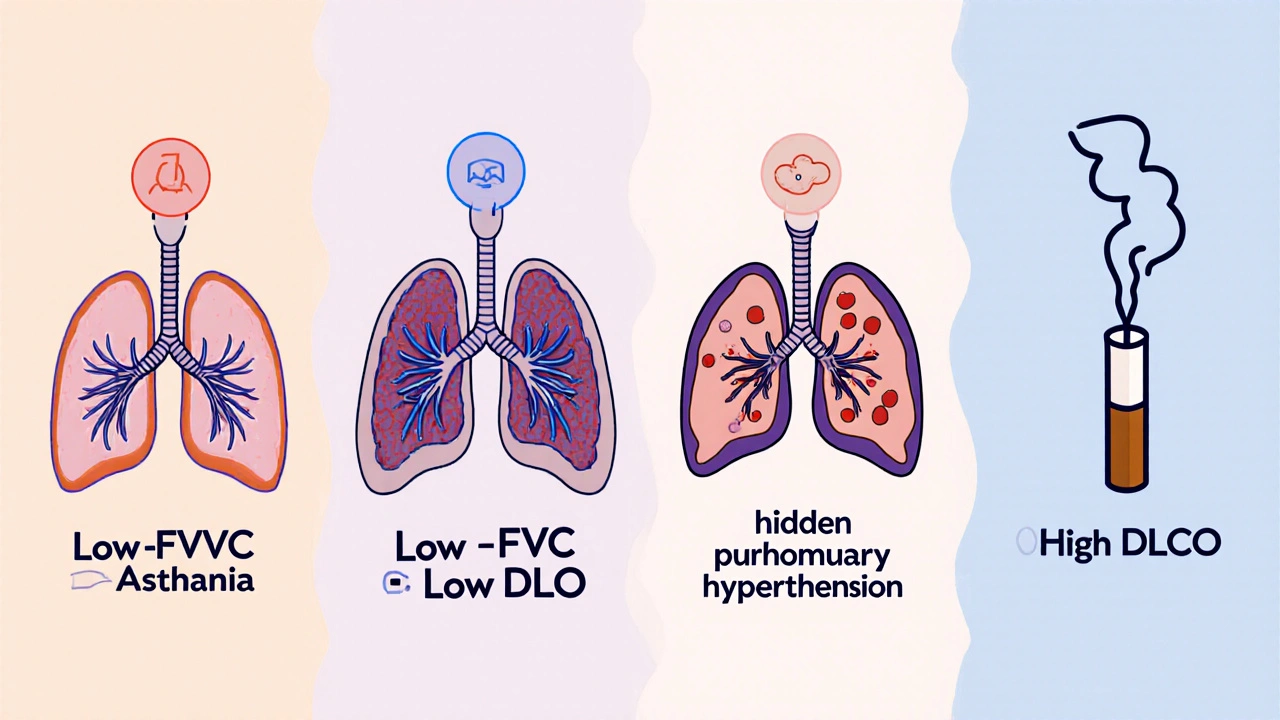
What to Do If Your Results Don’t Add Up
If your spirometry and DLCO seem contradictory, don’t panic. But do ask these questions:- Was my hemoglobin checked before the DLCO test?
- Did I avoid smoking for 24 hours before the test?
- Was the test done by someone trained in ATS/ERS standards?
- Are my results compared to the right reference values for my age, sex, and ethnicity?
The Future of Lung Testing
AI is starting to help. A 2023 study from Mayo Clinic showed algorithms that can predict pulmonary hypertension from DLCO patterns with 88% accuracy-better than many clinicians. That’s not replacing doctors. It’s giving them sharper tools. DLCO is also now a key measure in clinical trials for new fibrosis drugs. If a drug improves DLCO by 10%, it’s considered a meaningful win. That’s how important it’s become.Bottom Line
Spirometry tells you if your airways are blocked. DLCO tells you if your lungs can actually deliver oxygen to your body. One is about airflow. The other is about life. If you’re breathless and your spirometry is normal, don’t accept "it’s all in your head." Ask for a DLCO. If your DLCO is low, don’t ignore it. Dig deeper. Early detection of interstitial lung disease or pulmonary hypertension can change your trajectory-from decline to stability. These tests aren’t just numbers on a page. They’re clues. And when you know how to read them, you’re not just diagnosing a disease-you’re protecting your ability to breathe.What does a low DLCO mean if my spirometry is normal?
A low DLCO with normal spirometry suggests your lungs aren’t transferring oxygen into your blood properly-even though air can still move in and out. This is often an early sign of interstitial lung disease, pulmonary hypertension, or chronic blood clots in the lungs. It can also be caused by anemia, smoking, or high altitude. Further testing like a chest CT or echocardiogram is usually needed to find the exact cause.
Can I have COPD with a normal DLCO?
Yes. In early or mild COPD, especially chronic bronchitis, DLCO can remain normal because the problem is narrowed airways, not damaged lung tissue. But as emphysema develops, DLCO drops. A normal DLCO doesn’t rule out COPD-it just means the gas exchange part of your lungs is still working. If you’re a smoker with symptoms, don’t rely on DLCO alone.
Why is hemoglobin important for DLCO?
Carbon monoxide in the DLCO test binds to hemoglobin in your blood. If your hemoglobin is low (anemia), less CO can bind, making your DLCO appear lower than it really is. For every 1 g/dL drop in hemoglobin, DLCO falls by about 1%. That’s why labs must measure hemoglobin before testing and adjust the result-otherwise, you might get a false positive for lung disease.
Does smoking affect DLCO results?
Yes. Smoking raises levels of carbon monoxide in your blood, which competes with the test gas. This falsely lowers your DLCO by 5-10%. That’s why you’re told not to smoke for at least 24 hours before the test. Even secondhand smoke or vaping can interfere. If you smoked recently, your results may not be accurate.
Is DLCO testing painful or risky?
No. DLCO is completely non-invasive. You breathe in a small, harmless gas mixture (including carbon monoxide), hold your breath for 10 seconds, then exhale. The amount of CO used is less than what you’d get from smoking one cigarette. There’s no radiation, needles, or discomfort. The only challenge is holding your breath correctly-some older or very ill patients struggle with this.
How often should DLCO be repeated?
For stable conditions like COPD, DLCO is usually checked once a year-or if symptoms worsen. For progressive diseases like pulmonary fibrosis, it’s often done every 3-6 months to track how fast the disease is advancing. In clinical trials, it’s measured even more frequently. Your doctor will decide based on your diagnosis and treatment plan.
Can DLCO detect lung cancer?
Not directly. DLCO doesn’t show tumors. But if lung cancer blocks small airways or destroys lung tissue, it can lower DLCO. It’s not a screening tool for cancer, but a falling DLCO in someone with a lung mass might suggest the tumor is affecting gas exchange-which could influence treatment decisions.
What’s the difference between DLCO and lung volume tests?
Spirometry and DLCO don’t measure total lung size. For that, you need lung volume tests, like body plethysmography or helium dilution. These tests measure total lung capacity (TLC). If TLC is low, you have true restriction. If TLC is normal or high, your low FVC is likely due to air trapping (obstruction), not stiff lungs. DLCO helps explain why your lungs aren’t working-not how big they are.

Chris Vere
November 22, 2025 AT 04:15Interesting breakdown. I've seen patients with normal spirometry but constant fatigue and breathlessness. DLCO being the silent witness to underlying pathology is something I wish more clinicians took seriously. It's not just about airflow-it's about whether oxygen actually makes it into the bloodstream. The body doesn't care how much air you move if it can't use it.
Also, the hemoglobin point is critical. I've seen people misdiagnosed with ILD because their CBC wasn't checked. Iron deficiency isn't sexy, but it's common. Fix that first before ordering CTs.
Pravin Manani
November 23, 2025 AT 06:47From a pulmonary physiology standpoint, the FEV1/FVC ratio is the cornerstone of obstructive pattern recognition, but DLCO remains the gold standard for assessing alveolar-capillary membrane integrity. The diffusing capacity is governed by three primary variables: membrane thickness, capillary volume, and hemoglobin concentration. A depressed DLCO in the setting of preserved lung volumes suggests either interstitial thickening (fibrosis), microvascular destruction (emphysema), or reduced perfusion (PE).
Moreover, the 2023 Mayo AI study referenced is a landmark-machine learning algorithms now outperform human interpretation in detecting early pulmonary hypertension via DLCO slope analysis. This isn't the future-it's happening now in tertiary centers.
Sheldon Bazinga
November 23, 2025 AT 19:18bro why are we even doing this test if its so easy to mess up? i got my dlco done last year after i quit smoking and it was low. doc said "you got lung fibrosis". i was terrified. turns out i was still vaping and my hemoglobin was 10.5. they didn't even check it. this whole system is rigged. why do they charge $800 for a test that's wrong half the time? 🤡
Sandi Moon
November 25, 2025 AT 08:33Let me ask you this: How many of these "pulmonary function labs" are actually run by technicians who learned on YouTube? The ATS/ERS guidelines are clear-breath hold must be precisely 10 seconds, CO exposure must be calibrated, and hemoglobin correction is non-negotiable.
Yet I’ve seen clinics in the Midwest use 5-year-old machines, no calibration logs, and techs who don’t know what "predicted values" mean. This isn’t medicine. It’s a lottery. And when your DLCO comes back "low," you’re handed a prescription for steroids and sent away. Meanwhile, the real culprit? Undiagnosed pulmonary emboli. Or worse-corporate greed masking as healthcare.
Kartik Singhal
November 26, 2025 AT 02:04DLCO is just a fancy way to say "your lungs suck" 😒
Also, if you're a smoker, don't even bother. They'll just say "you have fibrosis" and charge you $5000 for a biopsy. I saw a guy on Reddit with a 58% DLCO and he turned out to be anemic. No one checks hemoglobin anymore. It's all AI and algorithms now. 🤖
Also, why do they always say "early interstitial disease"? That's just doctor code for "we don't know what's wrong but you're gonna pay for more tests."
Logan Romine
November 27, 2025 AT 04:13So let me get this straight…
You breathe in a tiny bit of poison (CO), hold your breath like you're trying to impress a girl at a pool party, and then-BOOM-you’re told your lungs are dying?
Meanwhile, your actual problem is you’re 30 pounds overweight, sleep 4 hours a night, and drink 3 energy drinks before bed.
DLCO doesn’t diagnose laziness. It diagnoses poor life choices. But hey, at least the bill is covered by insurance. 🙃
Leo Tamisch
November 28, 2025 AT 11:35There’s a profound metaphysical truth here: the body doesn’t lie. But the machines? They’re just mirrors reflecting our collective anxiety about mortality.
DLCO isn’t a number-it’s a mirror held up to the fragility of biological existence. We measure gas exchange because we’re terrified of suffocation-not just in lungs, but in meaning.
And yet, we treat it like a spreadsheet. We assign percentiles like they’re grades in school. But a DLCO of 62% isn’t a failure. It’s a whisper from your alveoli saying, "I’m still here. Don’t give up on me yet." We’ve forgotten that medicine is poetry disguised as science. This test doesn’t diagnose disease. It diagnoses the silence between breaths. And that silence? It’s the loudest thing in the room.
Shawn Sakura
November 29, 2025 AT 07:51This is one of the clearest, most helpful explanations I’ve ever read on pulmonary function testing. Seriously, thank you for taking the time to break this down like this.
As someone who’s worked in respiratory therapy for 18 years, I’ve seen too many patients dismissed because their spirometry looked "normal." DLCO is the unsung hero here. And yes-hemoglobin matters. Always check it.
If you’re breathless and your DLCO is low, don’t wait. Get a second opinion. Find a lab that follows ATS/ERS guidelines. You deserve accurate answers.
You’re not imagining it. Your lungs are talking. Listen.
And if you’re a smoker? Quit. Not for the test. For you.
Sammy Williams
December 1, 2025 AT 07:33My DLCO was 59% last year. Normal spirometry. Turned out I had mild pulmonary hypertension. Got on meds, started walking daily, and now it’s up to 72%. This test saved me. Don’t ignore it. Ask for it. Even if your doctor says "it’s fine."
Also-don’t smoke the day before. I did. Got a false low result. Had to redo it. Waste of time.