Pruritus in Cholestasis: Bile Acid Resins and New Treatment Options
 Jan, 19 2026
Jan, 19 2026
Itching that won’t go away-no rash, no bug bites, just relentless, deep skin irritation-is one of the most frustrating symptoms in liver disease. For people with cholestasis, where bile doesn’t flow properly from the liver, this itching isn’t just annoying. It can ruin sleep, wreck concentration, and make daily life unbearable. And here’s the twist: antihistamines, which work for most itchy skin conditions, do absolutely nothing for this type of itch. That’s because it’s not caused by histamine. It’s caused by bile acids and other molecules building up in the blood and triggering nerves in the skin. The good news? We now have clear, step-by-step ways to treat it-and newer options that actually work without the chalky taste or nasty side effects of older drugs.
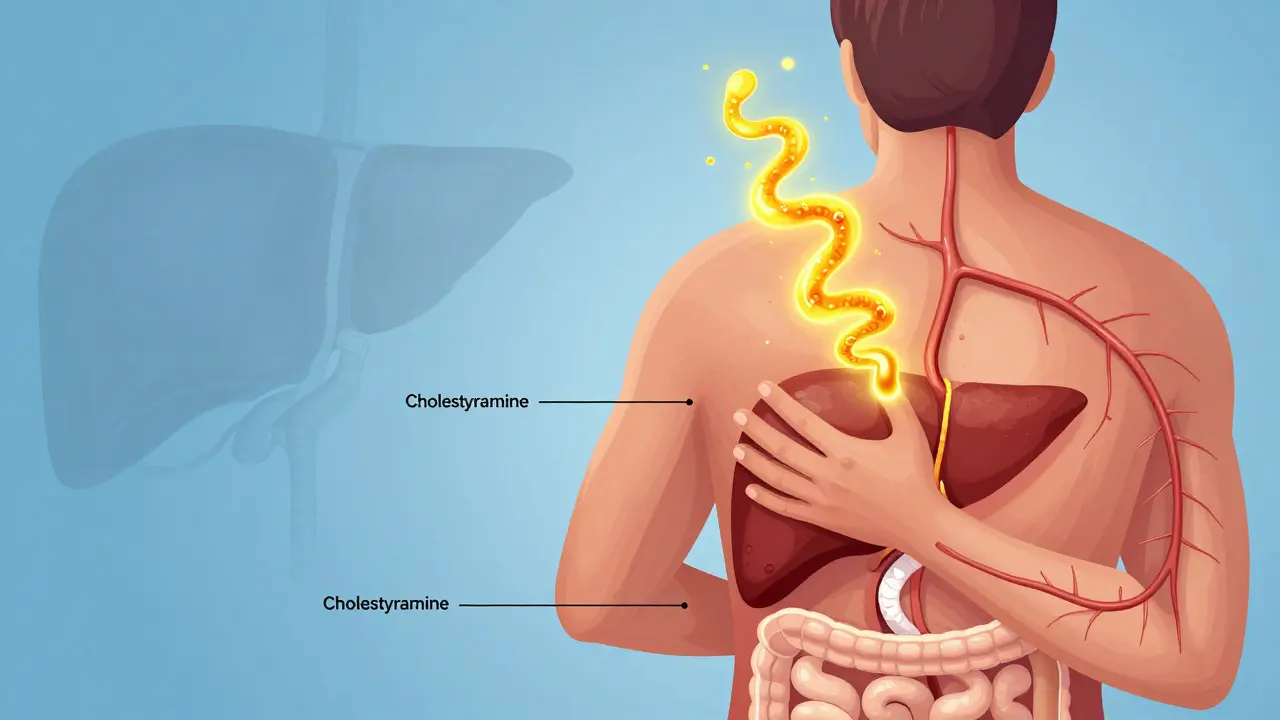
Why Bile Acid Resins Are Still the First Step
Cholestyramine (brand name Questran) has been the go-to treatment for cholestatic pruritus since the 1970s. It’s a bile acid resin-a powder that binds to bile acids in your intestines so they can’t be reabsorbed. Instead, they’re flushed out in your stool. Less bile acid in the blood means less itching. Studies show it works for 50 to 70% of patients, especially when the problem is caused by a blockage in the bile ducts. But here’s the catch: cholestyramine tastes like wet sand. A 2020 survey in Liver International found that 78% of patients couldn’t stand the texture. Many mix it with applesauce or juice to hide the grit, but even then, about a third quit within three months. The dose starts at 4 grams once a day, and your doctor will slowly increase it-up to 16 or even 24 grams daily-split into two or three doses. Timing matters too. You need to take it at least one hour before or four to six hours after any other medication, because it binds to pills too, including thyroid meds, blood thinners, and even birth control. Miss that window, and your other drugs won’t work right.When Cholestyramine Isn’t Enough: Rifampin Steps In
If you’ve tried cholestyramine for four weeks and your itching hasn’t dropped by at least half, it’s time to move to the next step: rifampin. This is an antibiotic you might know for treating tuberculosis, but at low doses (150 to 300 mg daily), it helps reduce itching in liver disease. How? It boosts liver enzymes that break down bile acids and other itch-causing substances. In people with primary biliary cholangitis (PBC), it works in up to 75% of cases. The downside? Rifampin turns your urine, sweat, and tears orange. It’s harmless but startling. Some patients report flu-like symptoms at first, and about 15 to 20% develop elevated liver enzymes, so your doctor will monitor your bloodwork closely. It also interacts with a lot of other drugs-over 50, including statins and antidepressants-because it speeds up how fast your liver breaks them down. Still, in clinical trials, rifampin has a lower discontinuation rate than cholestyramine. About 60 to 80% of patients see significant relief, and only 10 to 15% stop because of side effects.Naltrexone and Sertraline: Targeting the Brain’s Role in Itching
Itching in cholestasis isn’t just a liver problem-it’s a brain problem too. Research shows that bile acids activate opioid receptors in the spinal cord and brain, making the itch feel worse. That’s where naltrexone comes in. It’s an opioid blocker, originally used for alcohol and opioid addiction. At low doses (12.5 to 50 mg daily), it interrupts that signal. About 50 to 60% of patients report improvement, and it’s especially helpful for those who don’t respond to bile acid resins or rifampin. But getting started is rough. About 30% of patients feel like they’re going through opioid withdrawal in the first few days: nausea, anxiety, sweating, even insomnia. That’s why doctors start at just 6.25 mg and increase slowly, by 6.25 mg every week. If you can push through the first week, many find the itching drops sharply. Sertraline (Zoloft), an antidepressant, is used off-label for this too. It doesn’t work for everyone, but in PBC patients, studies show 40 to 50% get relief. It’s not clear why-maybe it affects serotonin pathways involved in itch signaling. It’s a good option if you’re also dealing with depression or anxiety, which is common in chronic liver disease. Dose is typically 75 to 100 mg daily. Unlike naltrexone, it doesn’t cause withdrawal-like symptoms, but it can take up to two weeks to start working.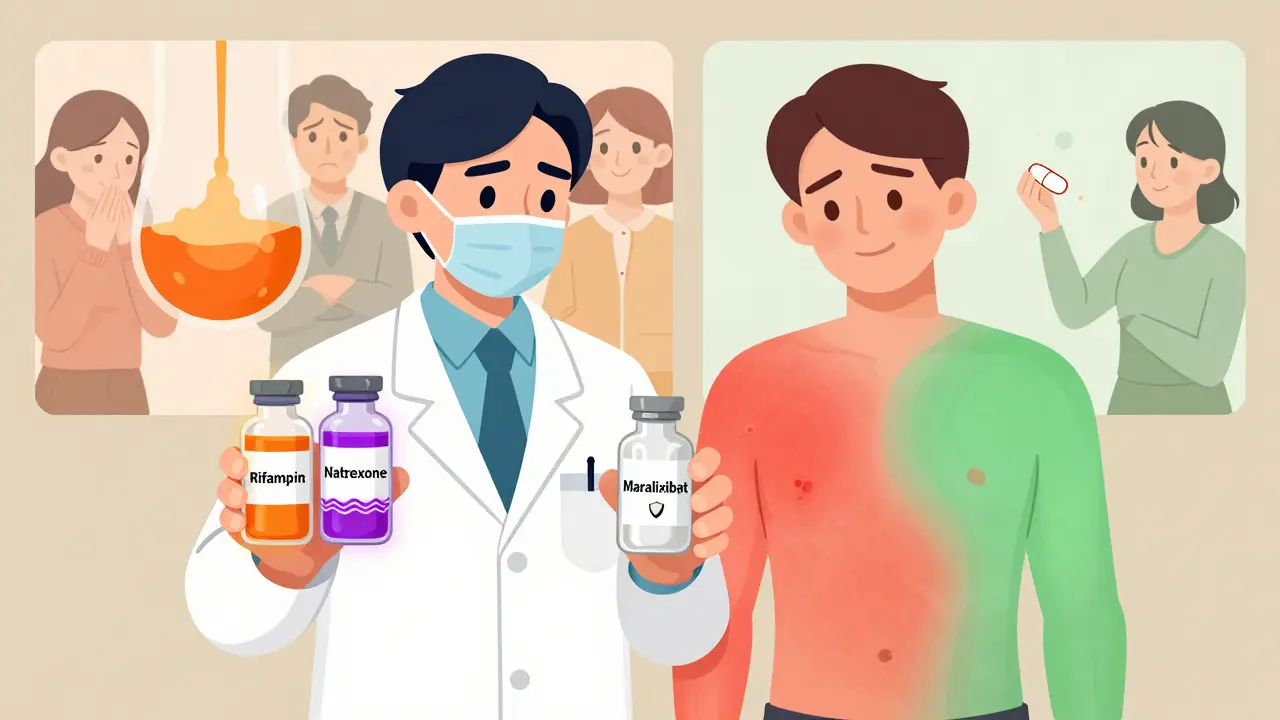
The New Wave: Maralixibat and Other Targeted Therapies
The biggest breakthrough in recent years isn’t a tweak of an old drug-it’s a completely new approach. Maralixibat (brand name Mytesi), approved by the FDA in 2021 for Alagille syndrome, blocks a protein in the intestine called IBAT. This stops bile acids from being recycled back into the blood. In clinical trials, it reduced itching by 47% on a standard scale, nearly matching cholestyramine-but with way fewer side effects. Only 12% of patients stopped taking it, compared to 35% for cholestyramine. Patients love it because it’s a once-daily pill with no taste. No grit. No orange urine. No drug interactions. A 2023 Cleveland Clinic survey showed 82% of patients kept taking it after six months. That’s huge. And it’s not alone. Volixibat, another IBAT inhibitor, showed 52% itch reduction in a 2023 trial. Both are now being studied for PBC and PSC, not just rare syndromes. Even more exciting are drugs targeting autotaxin and lysophosphatidic acid (LPA). Autotaxin is an enzyme that makes LPA, a molecule now known to be a major trigger of itch in cholestasis. In a 2023 phase 2 trial, an antisense drug called IONIS-AT332-LRx cut autotaxin levels by 65% and reduced itching by 58%. That’s more than double the effect of older drugs in some patients. These aren’t on the market yet, but they’re the future.What Doesn’t Work-and Why So Many Doctors Still Prescribe It
Despite decades of evidence, many primary care doctors still reach for antihistamines like hydroxyzine or diphenhydramine when a patient says they’re itchy. That’s because they assume all itching is the same. But cholestatic pruritus isn’t caused by histamine. Multiple studies, including AASLD’s 2022 guidelines, confirm antihistamines have no meaningful effect. A 2022 survey found 68% of primary care physicians still prescribe them first-despite guidelines saying not to. Other common but useless options include UV light therapy, topical corticosteroids, and herbal remedies. None have solid evidence. Even cool showers and moisturizers, while helpful for comfort, won’t stop the itch at its source. The key is targeting bile acids or the pathways they trigger.When Everything Else Fails: Transplant Is the Final Answer
For the 10 to 15% of patients who don’t respond to any medication, liver transplant is the only cure. And it works-95% of patients report their itching disappears completely after transplant. But it’s not a decision made lightly. It’s major surgery with lifelong risks. Most patients try every other option first. Still, knowing this is an option gives hope. For those with severe, unrelenting pruritus, transplant isn’t just about survival-it’s about getting back a normal life.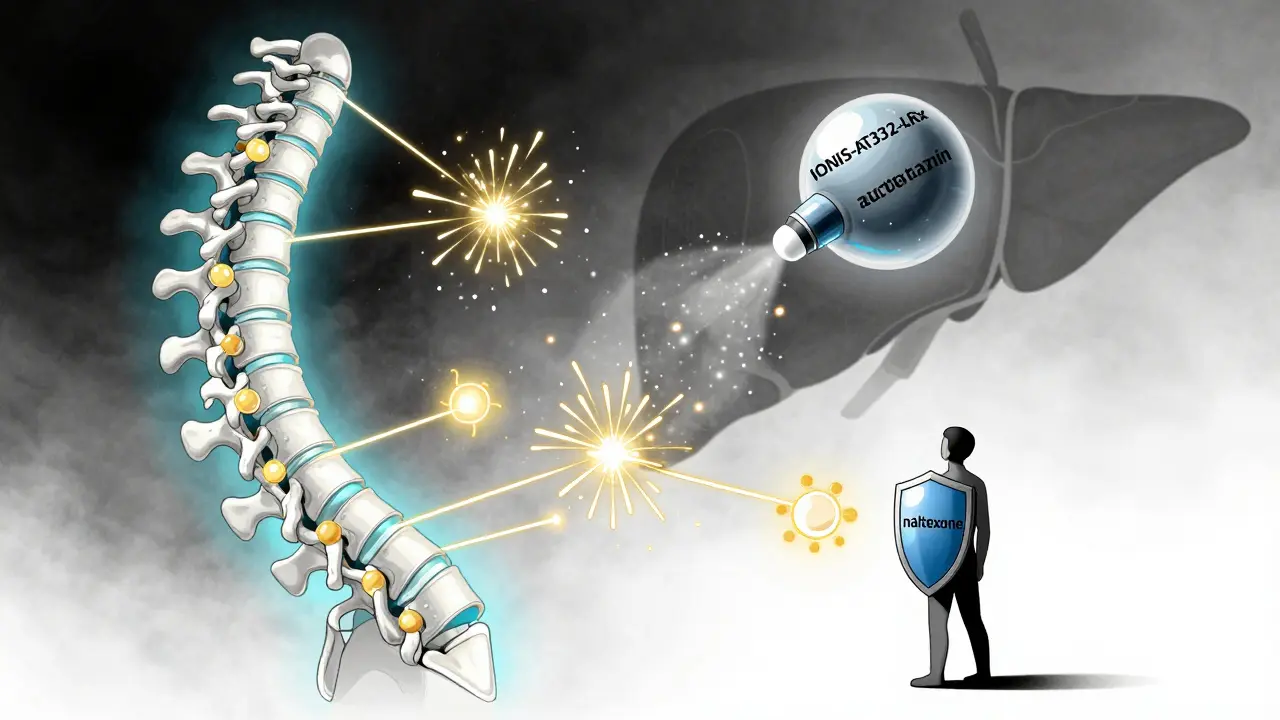
Practical Tips for Managing Cholestatic Itch Daily
While you’re working with your doctor on medication, small daily habits can help:- Take cool (not cold) showers-heat makes itching worse.
- Use fragrance-free moisturizers right after bathing.
- Wear loose, soft cotton clothes to avoid skin irritation.
- Keep fingernails short to prevent skin damage from scratching.
- Avoid hot tubs, saunas, and heavy exercise that raises body temperature.
- Use a humidifier at night if your skin feels dry.
Cost, Access, and the Real-World Gap
There’s a big gap between what works and what’s available. Maralixibat costs about $12,500 a month. Cholestyramine? $65. Insurance often blocks newer drugs unless you’ve tried the old ones first-and even then, approval can take months. A 2023 study found only 45% of community clinics follow the AASLD step-by-step guidelines. Most patients don’t have easy access to hepatologists. That means many are stuck on ineffective treatments for months or years. The good news? More insurance companies are starting to cover newer drugs as real-world data piles up. Patient advocacy groups are pushing for faster approvals. And with more phase 3 trials underway, we’re likely to see cheaper generics or biosimilars within the next few years.What’s Next? The Future of Itch Treatment
The next five years will change everything. We’re moving from treating symptoms to stopping the itch at its source. Drugs targeting autotaxin, LPA, and other specific pathways aren’t just experimental-they’re showing real results in trials. One day, instead of taking a chalky powder or a drug that turns your urine orange, you’ll take a pill that blocks the exact molecule causing your itch. That’s not science fiction. It’s already happening. For now, stick to the proven steps: start with cholestyramine, move to rifampin if needed, then try naltrexone or sertraline. Don’t give up if one drug doesn’t work-try the next. And if your doctor still prescribes antihistamines, ask why. You deserve better. The tools to truly help you are here. You just need to know how to ask for them.Why don’t antihistamines work for cholestatic itching?
Antihistamines block histamine, a chemical involved in allergic reactions and most skin rashes. But cholestatic pruritus is caused by bile acids and other molecules like lysophosphatidic acid (LPA) activating nerve pathways in the skin and spinal cord-not histamine. Multiple studies, including those from the American Association for the Study of Liver Diseases, show no meaningful benefit from antihistamines in this condition. Despite this, many doctors still prescribe them out of habit, because itching is commonly associated with allergies.
How long does it take for cholestyramine to start working?
Most people notice some relief within 3 to 7 days of starting cholestyramine, but it can take up to two weeks to see the full effect. Doctors usually recommend taking it for at least four weeks before deciding if it’s working. If there’s no improvement by then, it’s time to move to the next treatment step, like rifampin. Consistency matters-taking it at the same times each day and following the timing rules with other medications helps maximize its effectiveness.
Can I take cholestyramine with my other medications?
You can, but timing is critical. Cholestyramine binds to many drugs in the gut and stops them from being absorbed. To avoid this, take it at least one hour before or four to six hours after any other medication. This includes thyroid pills, blood thinners, antibiotics, birth control, and even vitamins. If you’re unsure, ask your pharmacist to review all your meds. Missing this window can make your other treatments ineffective.
Is maralixibat available for all types of cholestasis?
Currently, maralixibat is FDA-approved only for pruritus caused by Alagille syndrome. But it’s being studied in other forms of cholestasis, including primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC). Early results from phase 3 trials show similar effectiveness in these conditions. Many doctors prescribe it off-label for patients with PBC who can’t tolerate cholestyramine or rifampin. Insurance approval can be difficult, but patient advocacy and growing clinical evidence are helping expand access.
What are the side effects of rifampin for itching?
The most common side effect is orange discoloration of urine, sweat, and tears-it’s harmless but can be alarming. Some people get mild nausea, dizziness, or flu-like symptoms when starting. About 15 to 20% develop elevated liver enzymes, so blood tests are needed every few weeks. Rifampin also speeds up how fast your body breaks down other drugs, so it can reduce the effectiveness of birth control, blood thinners, and many other medications. Always tell your doctor about everything you’re taking before starting rifampin.
How do I know if my itching is from cholestasis?
Cholestatic itching usually starts on the palms and soles, then spreads. It’s often worse at night and not linked to a visible rash. Blood tests showing elevated alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) are key clues. If you have liver disease like PBC, PSC, or intrahepatic cholestasis of pregnancy, and you’re itchy without another explanation, cholestasis is likely the cause. A hepatologist can confirm this with blood tests and sometimes imaging. Don’t assume it’s eczema or dry skin-especially if you have a known liver condition.
Can lifestyle changes help with cholestatic itching?
Yes, but they’re supportive, not curative. Cool showers, fragrance-free moisturizers, loose cotton clothing, and avoiding heat can reduce irritation and make itching more manageable. Using a humidifier at night helps if your skin is dry. Avoiding alcohol and maintaining a healthy weight can also support liver function. However, these won’t reduce the bile acids causing the itch. They’re best used alongside medication-not instead of it.
Is liver transplant the only cure for severe cholestatic pruritus?
For patients who don’t respond to any medication, yes-liver transplant is the only treatment that reliably eliminates cholestatic pruritus. Studies show 95% of patients report complete or near-complete relief of itching after transplant. But it’s a major surgery with lifelong risks, including rejection and infection. Most patients try all medical options first. Transplant is considered when itching severely impacts quality of life, sleep, and mental health, and when other treatments have failed. It’s not just about survival-it’s about regaining a normal life.

Jerry Rodrigues
January 21, 2026 AT 08:45Cholestyramine tastes like sand mixed with regret. I took it for two weeks and quit. Rifampin turned my tears orange but at least I could sleep.
No more antihistamines. Ever.
Kelly McRainey Moore
January 21, 2026 AT 09:58I’ve been living with PBC for 8 years. Maralixibat changed my life. No grit, no orange, no drama. Just relief.
Wish I’d known about it sooner.
Ashok Sakra
January 22, 2026 AT 08:37why dont u just scratch it till it bleeds? that’s what i do. no meds needed. just tough it out. my liver dont care if i bleed.
stop being weak.
Amber Lane
January 23, 2026 AT 07:48My mom had cholestasis during pregnancy. The itching was unbearable. No one listened until she found a hepatologist.
Don’t ignore it. It’s not eczema.
michelle Brownsea
January 23, 2026 AT 11:00Let’s be honest: the pharmaceutical industry is profiting off suffering. Cholestyramine? A 1970s relic. Maralixibat? $12,500/month. And yet, the FDA approves it. Where’s the ethics?
They don’t want to cure you-they want you addicted to expensive, temporary fixes.
And don’t get me started on rifampin’s orange urine-another corporate gimmick to normalize bodily absurdity.
We’re being monetized, not healed.
Barbara Mahone
January 25, 2026 AT 10:21I’m a nurse in a liver clinic. I’ve seen patients cry from itching. I’ve seen them quit cholestyramine because they couldn’t swallow it.
Maralixibat is a miracle. But insurance denies it until the patient is suicidal.
That’s the system.
Stephen Rock
January 26, 2026 AT 17:51Everyone’s acting like this is groundbreaking. Newsflash: bile acids cause itch. We knew that in the 80s.
Now we have a pill that doesn’t taste like dirt? Groundbreaking.
Meanwhile, real science is out there-autotaxin inhibitors, LPA blockers-and you’re all cheering over a pill that costs more than my rent.
Pathetic.
Malvina Tomja
January 28, 2026 AT 00:30It’s not about the drugs. It’s about how we treat chronic illness as a personal failure.
You’re not weak for needing help. You’re not lazy for not ‘toughing it out.’
And you’re not crazy for wanting to live without constant, soul-crushing itching.
But the system? It’s designed to make you feel guilty for wanting relief.
Stop apologizing for needing treatment.
You deserve better.
Roisin Kelly
January 28, 2026 AT 18:25They say rifampin helps. But what if it’s just making your liver work harder? What if it’s causing damage we can’t see yet?
And what about the 20% who get elevated enzymes? Are they just collateral damage?
And why is no one talking about the fact that this whole treatment ladder is built on placebo-level evidence for half these drugs?
I’m not anti-medicine. I’m anti-bullshit.
MAHENDRA MEGHWAL
January 30, 2026 AT 00:22As a physician in rural India, I have witnessed patients with cholestatic pruritus suffering for months due to lack of access to even cholestyramine. The cost and logistics of newer therapies are unimaginable here.
Yet, we still see patients presenting with excoriated skin from scratching, misdiagnosed as dermatitis.
Education among primary care providers remains critically inadequate.
While novel agents like maralixibat represent progress, the true challenge lies in bridging the gap between clinical evidence and accessible care.
Until then, we rely on the simplest tools: cool compresses, cotton clothing, and compassion.
These are not luxuries-they are lifelines.
Samuel Mendoza
January 31, 2026 AT 23:55Wait-so the answer to itching is a liver transplant? That’s your endgame?
Why not just fix the bile ducts instead of burning the whole house down?
Transplant isn’t a cure-it’s a surrender.
And you’re telling people to take a pill that turns their tears orange before they even consider surgery?
That’s not medicine. That’s a delay tactic.
lokesh prasanth
February 1, 2026 AT 17:57maralixibat is just a fancy name for cholestyramine with better marketing. same thing, just more expensive. and the autotaxin stuff? still in trials. dont get your hopes up. we’ve been here before. they always say the next drug is the one. its never the one.
stick with what works. even if it tastes like sand.