Medicaid Substitution Rules: Mandatory vs Optional by State
 Nov, 12 2025
Nov, 12 2025
What Are Medicaid Substitution Rules?
Medicaid substitution rules exist to stop public health programs like Medicaid and CHIP from stepping in when a child already has access to affordable private insurance. These rules aren’t about denying care-they’re about making sure taxpayer dollars go to families who truly need them. Under federal law, states can’t use CHIP to replace private coverage that’s available and affordable. The goal? Keep private insurance strong while protecting public funds for those without other options.
The legal backbone comes from Section 2102(b)(3)(C) of the Social Security Act, updated in 1997 and again in 2010 under the Affordable Care Act. In March 2024, the Centers for Medicare & Medicaid Services (CMS) rolled out a major update to these rules, effective April 29, 2024. The new rule doesn’t scrap substitution rules-it fixes gaps. Now, states must make transitions between Medicaid and CHIP smoother, with fewer coverage lags.
Mandatory Rules: What All States Must Do
Every state running a CHIP program has to follow the same core rules. The biggest one: no substitution. That means if a child qualifies for affordable private insurance through a parent’s employer, CHIP can’t be used as a replacement. States must build systems to check whether private coverage exists and whether it’s affordable-meaning premiums don’t exceed 9.12% of household income in 2024, per IRS guidelines.
States also have to ensure smooth transitions. If a parent loses a job and their child loses private coverage, the state can’t make the family wait months to get on CHIP. The 2024 rule now requires automatic eligibility checks between Medicaid and CHIP programs. If a child’s income drops and they become eligible for CHIP, the system should switch them over without requiring a new application.
Another mandatory requirement: states must accept eligibility decisions from other federal programs like the Health Insurance Marketplace. If someone qualifies for premium tax credits, that counts as proof they’ve been screened for affordability. This cuts down on duplicate paperwork and speeds up enrollment.
Optional Rules: How States Choose to Enforce Substitution
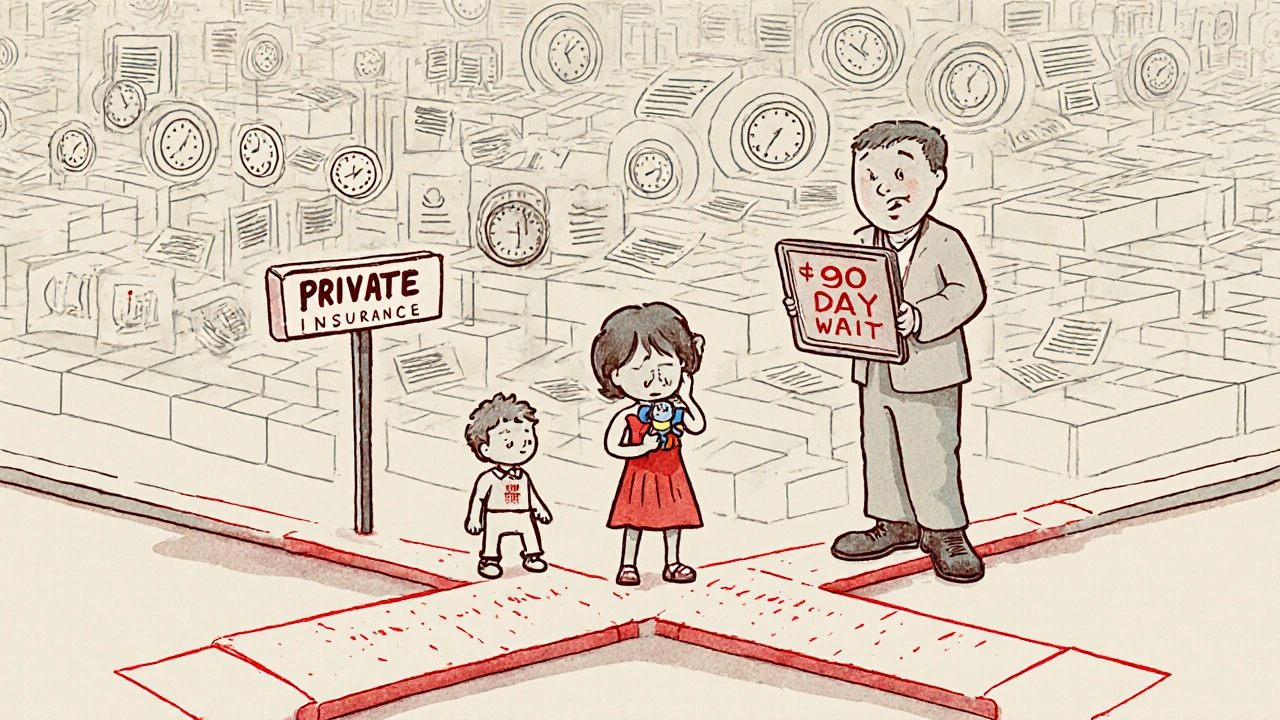
While the core rule is federal, states have flexibility in how they enforce it. The biggest optional tool? The 90-day waiting period. States can require families to wait up to 90 days before enrolling in CHIP if they’re believed to have access to private coverage. Thirty-four states use this method. Texas, California, and New York are among the largest to rely on it.
But here’s the catch: waiting periods don’t always work. In Ohio, a Medicaid worker described families losing coverage on Friday and needing CHIP by Monday-only to be denied for 12 weeks. Many end up uninsured. That’s why 15 states, including Florida, Illinois, and Pennsylvania, added extra exemptions. If a parent loses their job, has reduced hours, or experiences a family emergency, the waiting period can be skipped.
Other optional strategies include:
- Using real-time data to check private insurance status (28 states do this)
- Reliance on household surveys (22 states still use paper forms or phone interviews)
- Creating automated alerts when private coverage ends
- Building direct data links with employers or insurers
States with integrated Medicaid-CHIP systems-32 as of 2024-see 22% fewer coverage gaps than those with separate systems. Minnesota’s "Bridge Program" cut substitution-related gaps by 63% by connecting private insurer data directly to public eligibility systems. Louisiana, on the other hand, saw its uninsured child rate jump 4.7 percentage points after tightening verification in 2021.

Why States Struggle to Enforce These Rules
Enforcing substitution rules sounds simple. In practice? It’s messy. A 2023 survey of 47 state Medicaid agencies found that 68% listed "difficulty verifying private insurance" as their top challenge. Why? Because employers don’t always report coverage changes in real time. Some families decline coverage because they think it’s too expensive-then later can’t get on CHIP because the system still shows they had access.
Verification takes an average of 14.2 days. During that time, kids go without care. Parents get frustrated. A Families USA survey found 42% of families blamed "bureaucratic delays" for coverage gaps tied to substitution rules.
States also spend an average of $487,000 per year just to run verification systems. Smaller states with outdated tech struggle more. Only 19 states have comprehensive guidance for frontline workers. Twelve have materials so unclear, staff can’t apply the rules correctly.
And then there’s the problem of short-term insurance plans. These plans, which grew 78% from 2018 to 2023, don’t count as "affordable" under federal rules-but many families think they do. States have to figure out whether these plans meet the 9.12% affordability threshold, which adds another layer of complexity.
Real-World Impact: Who Gets Hurt?
Substitution rules were designed to protect public funds, but they sometimes hurt the people they’re meant to help. Working-class families with unstable jobs-like those in agriculture, hospitality, or seasonal work-are hit hardest. When their employer drops coverage mid-month, they can’t immediately qualify for CHIP. The 90-day wait becomes a gap in care.
Dr. Leighton Ku from George Washington University says the 90-day rule is outdated. "We designed it for a world where job changes happened once a year. Now, people switch jobs every few months. The rule doesn’t match reality."
Meanwhile, some states see the opposite problem: "churning." Parents drop their employer coverage just to get free CHIP. Texas administrators say this costs the state millions. That’s why some states keep strict rules-even if it means turning away families in need.
The result? In 2022, 21% of children experienced coverage gaps when moving between Medicaid and CHIP. States like Massachusetts, Minnesota, and Oregon-with real-time data sharing and automatic enrollment-got that number below 8%. The difference isn’t policy-it’s technology.

What’s Changing in 2025 and Beyond
The March 2024 rule forced states to start planning for better systems. By October 1, 2025, every state must have data-sharing protocols between Medicaid and CHIP. By December 31, 2025, they must accept eligibility decisions from the Health Insurance Marketplace.
Starting January 1, 2025, states must report quarterly on substitution-related metrics: how many kids had coverage gaps, how many waiting periods were used, how many exemptions were granted. This transparency will show which approaches work.
By 2027, experts predict all states will use automated data matching. Manatt Health forecasts a 65% drop in manual verification. That means fewer delays, fewer errors, and fewer kids falling through the cracks.
The Congressional Budget Office still sees substitution rules as cost-effective, saving $1.4 billion annually in inappropriate CHIP spending. But the Urban Institute warns: without modernization, these rules will lose effectiveness. By 2030, they could be 25% less useful as the insurance market keeps changing.
CMS Administrator Chiquita Brooks-LaSure said in May 2024 that the agency will review the first year of data and consider updates by late 2026. The goal isn’t to remove substitution rules-it’s to make them smarter.
What Families Should Know
If you’re a parent and your child loses private insurance, don’t assume you’re stuck waiting 90 days. Ask your state’s Medicaid office about exemptions. Job loss? Reduced hours? A family emergency? Those often qualify for immediate CHIP enrollment-even in states with waiting periods.
Also, don’t assume your employer’s plan is "affordable." If premiums take up more than 9.12% of your household income, your child may still qualify for CHIP. Many families miss this because they don’t know the rule exists.
And if you’re denied CHIP because of a substitution rule, ask for a written explanation. You have the right to appeal. Many denials are mistakes-wrong data, outdated records, or misapplied exemptions.
States vary wildly in how they handle this. In Minnesota, it’s automatic. In Louisiana, it’s a maze. Know your state’s rules. Call your local Medicaid office. Ask for their substitution policy guide. If they don’t have one, ask why.
Are Medicaid substitution rules the same in every state?
No. While all states must follow the federal rule that CHIP can’t replace affordable private insurance, how they enforce it varies. Thirty-four states use a 90-day waiting period, but 15 of those allow exemptions for job loss or reduced hours. Twenty-eight states use real-time data to check private coverage, while 22 still rely on paper forms or phone interviews. Some states have integrated Medicaid-CHIP systems that automatically switch kids between programs; others don’t.
Can a child be denied CHIP just because their parent has job-based insurance?
Only if that insurance is considered affordable-meaning the employee’s share of premiums doesn’t exceed 9.12% of household income in 2024. If the cost is too high, or if the parent declined coverage, the child can still qualify for CHIP. Many families are wrongly denied because states don’t verify affordability correctly. Always ask for a written explanation if you’re turned down.
What happens if I lose my job and my child loses private insurance?
You should qualify for immediate CHIP enrollment without waiting. Under the 2024 rule, losing employer coverage is a qualifying life event. States are required to process these cases quickly. If you’re told to wait 90 days, ask if your state offers an exemption for job loss. Most do. If they don’t, you can appeal the decision.
Do substitution rules make private insurance more expensive?
No. The rules are meant to prevent families from dropping private coverage to get free CHIP. If families did that, employers might stop offering coverage altogether. Substitution rules help keep private insurance stable by ensuring it remains the first option. Studies show states with strong substitution rules have lower rates of "churning"-where parents intentionally drop coverage to switch to CHIP.
Is there a way to avoid the 90-day waiting period?
Yes. Fifteen states allow exemptions for job loss, reduced work hours, divorce, death of a parent, or other hardships. Even in states that use waiting periods, you can request an exemption. You’ll need to provide documentation-like a termination letter or pay stub showing reduced income. If your state doesn’t have clear guidance, call their Medicaid office and ask for their substitution policy. You have rights under federal law.
What Comes Next?
The future of Medicaid substitution rules depends on technology-not politics. States that invest in real-time data sharing, automated transitions, and clear staff training will protect children’s coverage. Those that cling to paper forms and 90-day waits will keep seeing gaps.
If you’re a parent, know your rights. Ask questions. Don’t accept a denial without an explanation. If you’re a state worker, push for better systems. The tools exist-Minnesota showed it’s possible.
The goal isn’t to keep families off CHIP. It’s to make sure the right kids get help-when they need it, without unnecessary delays. The rules are changing. The question is: will your state keep up?

Johnson Abraham
November 13, 2025 AT 08:35Shante Ajadeen
November 13, 2025 AT 12:14dace yates
November 15, 2025 AT 04:11Danae Miley
November 15, 2025 AT 14:14Charles Lewis
November 17, 2025 AT 00:25Renee Ruth
November 18, 2025 AT 20:16Samantha Wade
November 19, 2025 AT 13:06Elizabeth Buján
November 21, 2025 AT 06:31Andrew Forthmuller
November 22, 2025 AT 23:40vanessa k
November 23, 2025 AT 23:07manish kumar
November 25, 2025 AT 10:59Nicole M
November 27, 2025 AT 10:12