Medex (Coumadin) vs Other Anticoagulants: Pros, Cons, and Best Alternatives
 Oct, 23 2025
Oct, 23 2025
Anticoagulant Decision Tool
Compare Anticoagulants
Answer a few questions to get a personalized recommendation based on your medical profile.
When choosing a blood‑thinner, Medex (Coumadin) is a vitamin K antagonist used to prevent clots in conditions like atrial fibrillation and deep‑vein thrombosis. It’s been on the market for decades, but newer drugs have entered the scene, promising fewer doctor visits and fewer diet restrictions. If you’re weighing whether to stay on Medex or switch, this guide breaks down the facts, compares the biggest alternatives, and helps you decide what fits your life best.
Key Takeaways
- Medex (Coumadin) requires regular INR monitoring, while most newer anticoagulants do not.
- Newer options-Xarelto, Eliquis, Pradaxa-offer fixed dosing and fewer food interactions.
- Patients with severe kidney disease or mechanical heart valves may still need Medex.
- Cost varies: generic warfarin is cheap, but insurance often covers NOACs better in 2025.
- Switching should always involve your prescriber; abrupt changes can raise clot‑risk.
What Is Medex (Coumadin)?
Medex is the brand name for warfarin, a synthetic compound that blocks vitamin K recycling. Vitamin K is essential for clotting factor production, so when you block it, your blood stays thinner. The drug is prescribed for three main reasons:
- Preventing stroke in atrial fibrillation patients.
- Treating or preventing deep‑vein thrombosis (DVT) and pulmonary embolism (PE).
- Managing patients with mechanical heart valves.
Because warfarin’s effect can swing widely based on diet, other meds, and genetics, doctors track its activity using the international normalized ratio (INR). The target INR range is usually 2.0‑3.0, but it can differ for specific conditions.
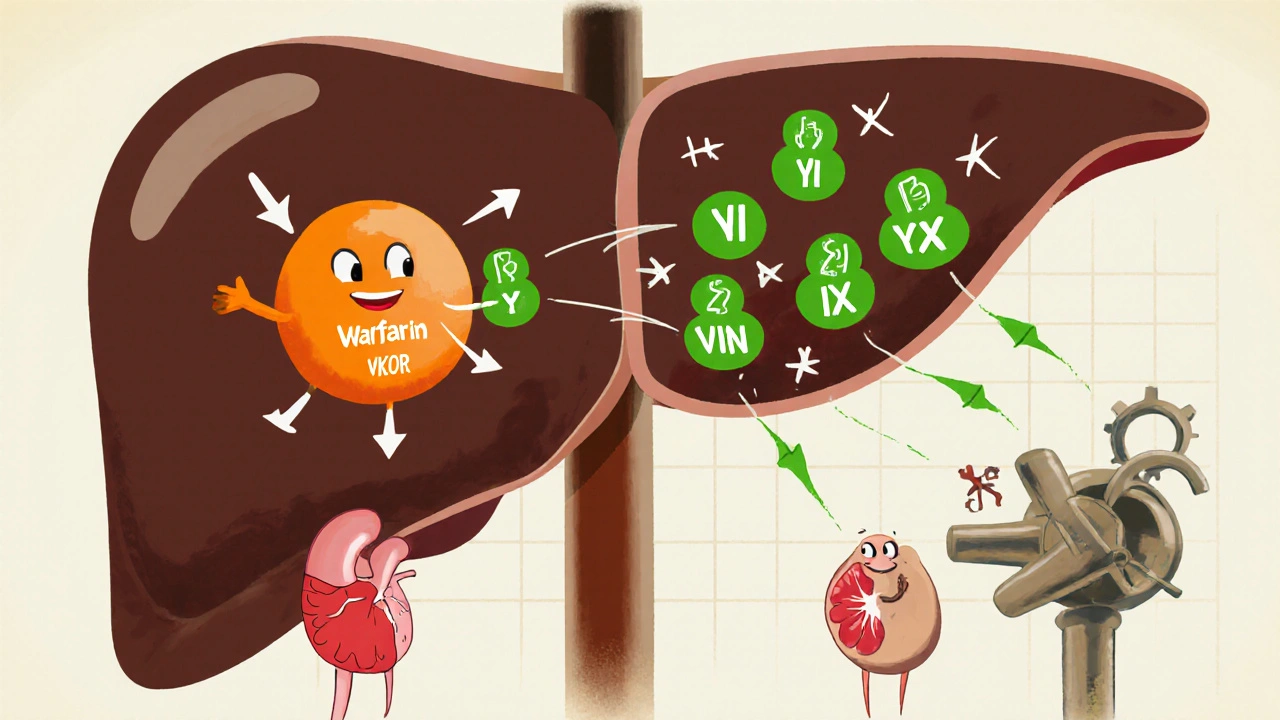
How Does Medex Work? (A Simple Breakdown)
Warfarin binds to an enzyme called vitamin K epoxide reductase (VKOR). This stops the liver from converting inactive vitamin K epoxide back to its active form. Without active vitamin K, the liver can’t add a crucial side‑chain to clotting proteins (II, VII, IX, and X). Those proteins stay “inactive,” so clots form more slowly.
Because the pathway involves many steps, the drug’s effect builds up over a few days. That’s why doctors start patients on a low dose and adjust slowly based on INR readings.
Who Typically Takes Medex?
In 2025, roughly 1.5 million adults in the United States still use warfarin, according to the National Heart, Lung, and Blood Institute. The typical user profile includes:
- People over 65 with atrial fibrillation.
- Patients who have already experienced a DVT or PE.
- Individuals with a mechanical mitral valve - the only condition where newer direct oral anticoagulants (DOACs) are not approved.
For many, the biggest hassle is weekly or bi‑weekly blood draws to keep INR in range.
Major Drawbacks of Medex
- Frequent monitoring: INR checks are required at least once a month, sometimes more.
- Dietary restrictions: leafy greens, vitamin K‑rich foods can shift INR dramatically.
- Drug interactions: antibiotics, antifungals, and even over‑the‑counter supplements can raise bleeding risk.
- Variable dosing: genetic factors (CYP2C9, VKORC1) mean two patients may need very different doses.
- Bleeding risk: While effective, warfarin’s narrow therapeutic window increases the chance of serious bleeding if INR spikes.
Enter the New Kids: Direct Oral Anticoagulants (DOACs)
In the last decade, four DOACs have become mainstream. They target specific steps in the clotting cascade, allowing fixed dosing and eliminating routine INR testing.
Xarelto (rivaroxaban) inhibits factor Xa directly.
Eliquis (apixaban) also blocks factor Xa but has a slightly lower bleeding profile.
Pradaxa (dabigatran) is a direct thrombin (factor IIa) inhibitor.
All three are taken once (Xarelto) or twice daily (Eliquis, Pradaxa) with no need for routine blood work.
Comparison Table: Medex vs. Major Alternatives
| Feature | Medex (Coumadin) | Xarelto (Rivaroxaban) | Eliquis (Apixaban) | Pradaxa (Dabigatran) |
|---|---|---|---|---|
| Drug class | Vitamin K antagonist | Factor Xa inhibitor | Factor Xa inhibitor | Direct thrombin inhibitor |
| Monitoring | INR checks required | No routine labs | No routine labs | No routine labs |
| Frequency | Once daily (dose adjusted) | Once daily with food | Twice daily | Twice daily |
| Kidney safety | Safe down to CrCl 30 ml/min | Contraindicated < 15 ml/min | Contraindicated < 15 ml/min | Contraindicated < 30 ml/min |
| Reversal agent | Vitamin K, PCC | Andexanet alfa (limited) | Andexanet alfa | Idarucizumab (specific) |
| Typical daily cost (US) | $4 (generic) | $12‑$15 | $13‑$16 | $14‑$17 |
| Approved for mechanical heart valve | Yes | No | No | No |
When to Stay on Medex (Coumadin)
Even with the convenience of DOACs, Medex remains the best choice in a few scenarios:
- Mechanical heart valves: Clinical trials showed higher clot risk with DOACs.
- Severe chronic kidney disease (CKD stage 4‑5): Warfarin can be dose‑adjusted safely.
- Cost‑sensitive patients without good insurance: Generic warfarin is often the cheapest option.
- Patients already well‑controlled on warfarin: Switching may destabilize INR and increase risk.
When to Consider a DOAC
If you’re tired of weekly blood draws, have a stable diet, and meet the kidney criteria, a DOAC can improve quality of life. Here’s a quick decision matrix:
| Patient Profile | Best Choice | Why |
|---|---|---|
| Atrial fibrillation, normal kidney function, wants fewer lab visits | Eliquis | Lowest major bleeding risk among DOACs |
| Recent DVT, prefers once‑daily dosing | Xarelto | Convenient once‑daily schedule |
| History of gastrointestinal bleeding | Pradaxa | Lower GI bleed rates compared to rivaroxaban |
| Severe CKD (eGFR 20‑30 ml/min) | Medex (Coumadin) | Warfarin dosing can be safely adjusted |
How to Switch Safely
Never stop warfarin cold. Your doctor will typically use a “bridging” plan:
- Check your INR; ensure it’s below 2.0.
- Stop Medex and start the chosen DOAC at a dose based on your kidney function.
- Schedule a follow‑up lab 2‑4 days later to confirm no residual anticoagulant effect.
- Watch for signs of bleeding (bruises, hematuria) or clotting (leg pain, shortness of breath).
Most patients feel the switch is painless, but the first week is critical for monitoring.
Frequently Asked Questions
Is Medex the same as warfarin?
Yes. Medex is a brand name for the generic drug warfarin, which works by blocking vitamin K.
Do DOACs need any blood monitoring?
Generally no. Unlike warfarin, DOACs are given at fixed doses and don’t require routine INR checks.
Can I take Medex if I’m pregnant?
Warfarin crosses the placenta and can cause fetal abnormalities, so it’s usually avoided. Heparin is preferred during pregnancy.
What’s the antidote if I bleed while on a DOAC?
Eliquis and Xarelto can be reversed with andexanet alfa (available in hospitals). Pradaxa has a specific antidote called idarucizumab.
Is it cheaper to stay on warfarin?
The drug itself is cheap, but the cost of frequent INR labs and clinic visits can add up. Many insurers now cover DOACs, making the total cost comparable.
Bottom Line
Medex (Coumadin) still saves lives, especially for patients with mechanical heart valves or severe kidney disease. For most others, the newer NOACs-Xarelto, Eliquis, Pradaxa-offer a simpler, more predictable experience. The right choice boils down to your medical history, kidney function, insurance coverage, and how much you mind regular blood tests.
Talk with your healthcare provider, weigh the pros and cons, and don’t rush the switch. Your safety is worth the conversation.

Naomi Shimberg
October 23, 2025 AT 13:14While the article extols the virtues of the newer direct oral anticoagulants, it neglects to acknowledge the profound historical significance of warfarin, known here as Medex, in the annals of hematology. One must consider that the very existence of modern anticoagulation theory rests upon the paradigmatic discoveries made with vitamin‑K antagonism. The author’s implication that warfarin is merely an antiquated inconvenience betrays a myopic focus on convenience over safety. Clinical experience has demonstrated that the predictability of warfarin dosing, when meticulously monitored, can outweigh the marginal benefits of a DOAC in patients with fluctuating renal function. Furthermore, the cost analysis presented fails to factor in the long‑term economic burden of emergency reversals necessitated by DOAC‑related bleeding. Institutions that have retained warfarin protocols often report lower incidence of catastrophic hemorrhage due to the availability of well‑established reversal agents such as vitamin K and prothrombin complex concentrates. It is also a disservice to patients with mechanical heart valves to suggest a blanket transition to DOACs, given the robust data indicating increased thrombotic events in this cohort. The narrative subtly encourages a wholesale abandonment of a drug that has saved countless lives, an agenda that seems at odds with the principle of evidence‑based medicine. A contrarian perspective obliges us to scrutinize the underlying motivations, including pharmaceutical lobbying that may be influencing the promotional tone of the piece. Moreover, the purported convenience of fixed dosing overlooks the reality that patient adherence to a twice‑daily regimen, as required by many DOACs, can be more challenging than a once‑daily warfarin schedule. The article’s omission of the nuanced role of genetics in warfarin metabolism further illustrates an incomplete appraisal. When evaluating therapeutic options, one must weigh both the biochemical mechanisms and the psychosocial impacts of frequent monitoring, which for many patients offers a reassuring touchpoint with their healthcare provider. In sum, the reductionist view that newer equals better is not universally applicable. Warfarin, despite its age, remains a versatile, cost‑effective, and clinically validated agent for a substantial subset of the anticoagulated population. Therefore, I urge clinicians to adopt a balanced, patient‑centered approach rather than capitulating to a trend that may be driven more by market forces than by indisputable clinical superiority.
Zachary Blackwell
October 27, 2025 AT 13:28Yo, ever wonder why the pharma giants push those shiny DOAC pills like they're the cure‑all? 🤔 They keep the warfarin clinics quiet so they can rake in the profits from all those lab fees. I’m telling ya, the real story is hidden behind glossy ads and a sea of “convenient” promises. Stay skeptical, folks.
Shubhi Sahni
October 31, 2025 AT 11:54Indeed, the historical context you invoke is indispensable; however, let us also recognize that patient education programs have evolved substantially, and modern INR monitoring devices are now user‑friendly, even home‑based, offering real‑time feedback; this mitigates the inconvenience you describe, and fosters autonomy. Moreover, the cost dynamics you highlight can be offset by insurance formularies that now cover DOACs at reduced copays, a fact often omitted in traditional narratives! Nevertheless, marrying the legacy of warfarin with contemporary therapeutic strategies could yield a synergistic paradigm, one that respects both safety and quality of life.
Danielle St. Marie
November 4, 2025 AT 07:34Only Americans truly appreciate the reliability of a tried‑and‑true blood thinner like Medex-no need for fancy foreign drugs! 🇺🇸💊
keerthi yeligay
November 8, 2025 AT 00:28I think the article missed the point that not every patient can afford the fancy meds, its a real issue. Simpler is often better.
Peter Richmond
November 11, 2025 AT 14:34Your observation underscores a crucial socioeconomic dimension; clinicians must indeed tailor anticoagulation strategies to individual financial circumstances, ensuring equitable access without compromising therapeutic efficacy.
Bonnie Lin
November 15, 2025 AT 01:54Warfarin's track record is solid-no need for hype.
sara fanisha
November 18, 2025 AT 10:28Totally! If it works, why mess with it? Keep it simple and stay safe.
Tristram Torres
November 21, 2025 AT 16:14Warfarin is boring and hard to keep track of, but the new pills are not perfect either.
Jinny Shin
November 24, 2025 AT 19:14Alas, the tragedy of the ordinary! While we crave simplicity, the shadow of bleeding looms over every choice, and the stage of our veins knows no mercy!
deepak tanwar
November 27, 2025 AT 19:28One might argue that the author’s enthusiasm for DOACs neglects the intricate pharmacogenomic interplay that renders warfarin a uniquely adaptable agent; consequently, dismissing it outright may deprive certain patients of a precisely calibratable therapy.
Abhishek Kumar
November 30, 2025 AT 16:54Meh, both options seem overhyped.
hema khatri
December 3, 2025 AT 11:34Wow! This debate is fire! You all forget that Medex has saved millions-no joke! Let’s not dismiss the old guard!!
Jennell Vandermolen
December 6, 2025 AT 03:28I appreciate everyone’s perspectives; perhaps the best path is a shared decision model where clinicians discuss risks, benefits, and personal preferences with patients before committing to any anticoagulant regimen.
Mike Peuerböck
December 8, 2025 AT 16:34What a vibrant tapestry of opinion we have woven here-each thread adds depth to our collective understanding yet we must anchor our choices in rigorous evidence and patient‑centered care.