Liver Cancer Risk After SVR: Why Surveillance Still Matters
 Dec, 15 2025
Dec, 15 2025
When you hear that hepatitis C has been cured, it’s easy to think the danger is over. After all, the virus is gone. Your liver is healing. You feel better than you have in years. But here’s the truth: liver cancer risk after SVR doesn’t vanish - not even close.
Sustained Virologic Response (SVR) means the hepatitis C virus is undetectable 12 or 24 weeks after treatment ends. That’s a cure. Direct-acting antivirals (DAAs) have made this possible for more than 95% of patients since 2014. But curing the virus doesn’t mean your liver goes back to being a healthy, young liver. If you had advanced scarring - fibrosis or cirrhosis - before treatment, your risk of liver cancer remains real.
What SVR Actually Changes - and What It Doesn’t
SVR cuts your risk of hepatocellular carcinoma (HCC), the most common type of liver cancer, by about 71%. That’s huge. Compared to people who never got treated, your chances of developing cancer drop dramatically. But that doesn’t mean you’re safe.
Think of it like quitting smoking. Your lung cancer risk goes way down, but if you smoked for 30 years, your risk never returns to the level of someone who never smoked. The same applies to your liver. Years of inflammation and scarring leave behind changes that can still lead to cancer, even without the virus.
Studies show that among patients with cirrhosis who achieved SVR, the annual rate of liver cancer is still around 2.1 to 2.3 cases per 100 people. That’s lower than the 4.5 cases per 100 in untreated cirrhotic patients - but it’s still high enough to warrant attention. For context, the average person without liver disease has a risk of less than 0.1 per 100 per year.
The Real Danger: Advanced Fibrosis and Cirrhosis
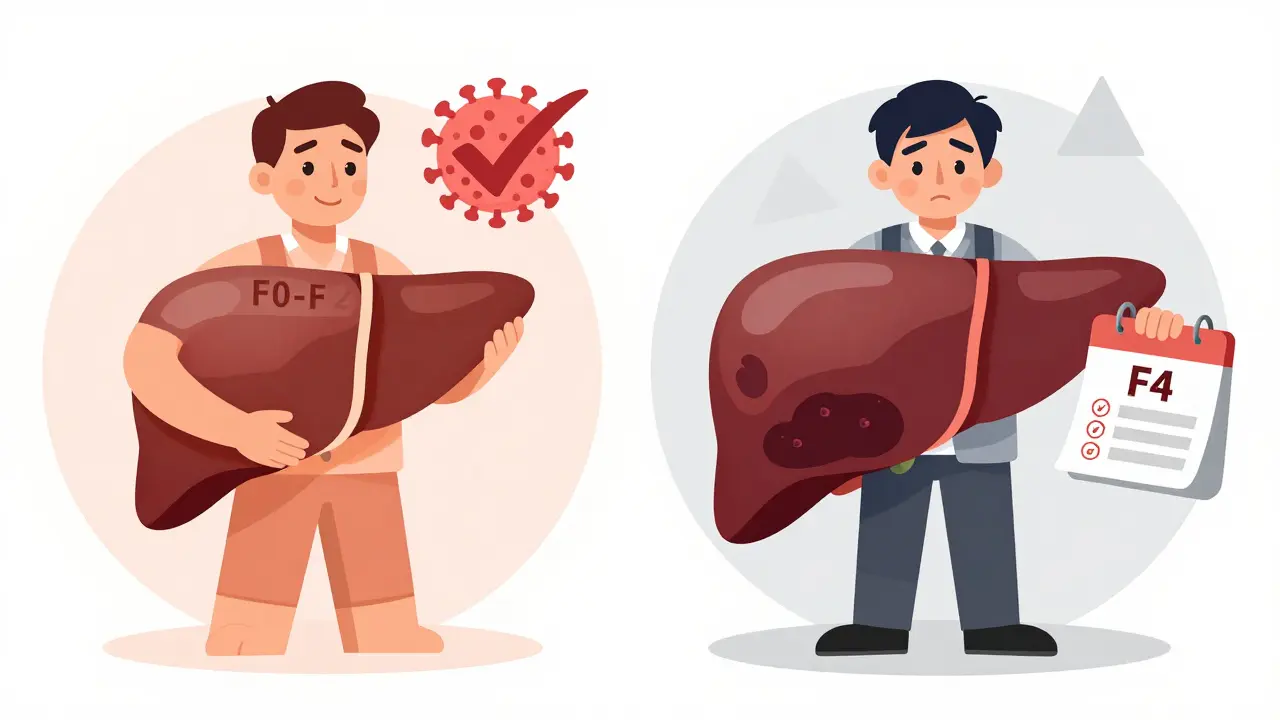
Not everyone who had hepatitis C is at equal risk. The biggest predictor of ongoing cancer risk is how much scarring your liver had before treatment.
- If you had cirrhosis (F4) before treatment: your risk remains high. Surveillance is non-negotiable.
- If you had advanced fibrosis (F3): you’re in a gray zone. Some guidelines say yes to surveillance, others say no.
- If you had mild or no fibrosis (F0-F2): your risk is extremely low. You likely don’t need ongoing screening.
Doctors use tools like FibroScan (transient elastography) and the FIB-4 index to measure liver stiffness. After SVR, if your FibroScan reading is above 11.2 kPa, or your FIB-4 score stays above 3.25, your cancer risk doesn’t drop to zero. These numbers aren’t guesses - they’re backed by data from thousands of patients tracked over years.
A 2024 review in the Journal of Clinical and Translational Hepatology confirmed that these tools predict cancer risk better than any other method available today. They’re not perfect, but they’re the best we have.
The Global Divide in Guidelines
Here’s where things get messy. Different countries give different advice.
In Europe, the European Association for the Study of the Liver (EASL) says: “If you had F3 or F4 fibrosis before treatment, keep getting screened every six months.” They’re worried that doctors might miss early cirrhosis. They’d rather over-screen than miss a cancer.
In the U.S., the American Association for the Study of Liver Diseases (AASLD) says: “Only screen if you have cirrhosis (F4). F3 patients don’t need it.” Their argument? The absolute risk in F3 is too low to justify the cost and anxiety of regular scans.
Both sides have data. But the truth is, we’re still learning. Some patients with F3 fibrosis see their scarring improve after SVR. Others don’t. And cancer can still develop - even in people who were told they were “low risk.”
Dr. Anna Lok, former president of AASLD, has said she stands by the U.S. guidelines. But Dr. Markus Peck-Radosavljevic, a leading EASL expert, argues that ultrasound is cheap, non-invasive, and the cost of missing one cancer is too high. He’s not wrong.
Why So Many People Stop Screening - and Why That’s Dangerous
Here’s the biggest problem: most people stop getting screened after SVR.
A 2023 JAMA study found that only about 25% of eligible patients get the recommended twice-yearly ultrasounds. That’s not because they’re careless. It’s because they think they’re cured. They feel fine. Their doctor doesn’t bring it up. They’re told, “The virus is gone,” and they assume everything else is fixed too.
Patients often don’t realize that their liver still needs monitoring. Clinicians, overwhelmed with appointments, may assume the patient knows. Or worse - they assume the guidelines say “no screening needed” and don’t double-check the patient’s fibrosis stage.
And here’s the kicker: people who’ve been through hepatitis C treatment are more likely to drop out of care. They’ve fought a long battle. They’re tired. They want to move on. But that’s exactly when they’re most vulnerable.
What You Should Do - Step by Step
If you’ve achieved SVR, here’s what you need to do right now:
- Find out your fibrosis stage before treatment. Ask your doctor for your FIB-4 score or FibroScan result. If you don’t know, get it checked.
- If you had cirrhosis (F4): schedule a liver ultrasound every six months. Add an AFP blood test if your doctor recommends it.
- If you had advanced fibrosis (F3): talk to your doctor. Ask if you should be screened. Don’t accept “it’s not necessary” without seeing your numbers.
- If you had mild or no fibrosis (F0-F2): you likely don’t need screening, but get a baseline liver check-up every 1-2 years.
- Keep your liver healthy. Avoid alcohol. Manage your weight. Control diabetes if you have it. These things matter - even after SVR.
Don’t wait for symptoms. Liver cancer often has none until it’s advanced. By then, treatment options are limited.
What’s Next? The Future of Surveillance
Researchers are working on better tools. A new blood test called the GALAD score - which looks at gender, age, and three protein markers - can detect early cancer with 85% accuracy. It’s not yet standard, but it’s coming.
Some hospitals are using AI to analyze ultrasound images for subtle signs of cancer. Others are testing dynamic risk models that adjust screening frequency based on how your liver changes over time. If your FibroScan drops below 9.5 kPa after SVR, you might be able to stretch your scans to once a year - or even every 18 months.
But for now, the safest path is clear: if you had advanced scarring, keep getting screened. It’s simple. It’s cheap. And it saves lives.
Final Thought: Cure Doesn’t Mean Clean Slate
SVR is a triumph. It’s one of the greatest medical advances of the last decade. But it’s not the end of the story.
Your liver remembers. And if it was damaged before, it still needs protection. Don’t let the success of your treatment make you careless. Keep your appointments. Ask the hard questions. Stay vigilant.
Because after all you’ve been through, the last thing you want is to let liver cancer sneak in - not because the virus came back, but because you stopped watching.
Do I still need liver cancer screening after being cured of hepatitis C?
Yes - if you had advanced fibrosis (F3) or cirrhosis (F4) before treatment. Even after the virus is gone, your liver may still be at risk for cancer. Screening with ultrasound every six months is recommended for these patients. If you had mild or no scarring, your risk is very low and routine screening is usually not needed.
Is liver cancer risk the same after DAA treatment versus interferon?
The risk reduction is similar, but slightly different. Studies show DAA-only treatment reduces HCC risk by about 71%, with a hazard ratio of 0.29. Interferon-based treatment reduces risk by about 68% (HR 0.32). The key point is that both treatments lower risk dramatically, but neither eliminates it - especially if you had cirrhosis before treatment.
What if my FibroScan improved after treatment? Do I still need screening?
Improvement is good news, but it doesn’t automatically mean you’re safe. If your pre-treatment FibroScan was above 12.6 kPa (indicating cirrhosis), you still need screening even if it’s now below 11.2 kPa. If you had advanced fibrosis (F3) and your post-SVR FibroScan is under 9.5 kPa, you may be able to reduce screening frequency - but only under a doctor’s supervision.
Why do European and American guidelines differ on screening after SVR?
Europe recommends screening for both F3 and F4 patients because they worry about misclassifying cirrhosis and believe the cost of ultrasound is low compared to the risk of missing cancer. The U.S. only recommends screening for F4 patients because studies show the absolute cancer risk in F3 is very low, and they want to avoid unnecessary testing. Both positions are supported by data - it’s a difference in risk tolerance, not medical evidence.
Can I stop screening if I’ve been cancer-free for 5 years after SVR?
Current guidelines say no - especially if you had cirrhosis. The risk declines over time, but it doesn’t disappear. Some studies suggest that after 5-7 years with no cancer and stable fibrosis, screening intervals might be extended, but this is still under research. Never stop screening without discussing it with your hepatologist.

Thomas Anderson
December 16, 2025 AT 18:58Just got SVR last year and was totally clueless about needing screenings. My doc never mentioned it. Glad I found this - going to schedule my ultrasound this week.
Daniel Wevik
December 17, 2025 AT 14:00SVR is a milestone, not a finish line. The 71% risk reduction is statistically significant, but the residual hazard in F3/F4 patients remains clinically relevant. Persistent epigenetic dysregulation, altered hepatic stellate cell phenotype, and microenvironmental fibrotic niches continue to drive oncogenic pathways independent of viral replication. Surveillance isn't optional - it's a biological imperative.
Rulich Pretorius
December 19, 2025 AT 00:38This is the kind of post that saves lives. I’m from South Africa where access to FibroScan is still limited, but even basic ultrasound screening every six months is better than nothing. If you’ve had HCV and had any scarring - don’t stop now. Your future self will thank you.
Alexis Wright
December 20, 2025 AT 11:03Let’s be real - the American liver guidelines are a joke. They’re not based on science, they’re based on insurance company spreadsheets. You want to save money? Fine. But don’t pretend it’s about patient care when you’re letting people with F3 fibrosis walk into cancer blind. The data says F3 carries risk. The guidelines ignore it. That’s not medicine - that’s negligence dressed up as cost-efficiency.
Dwayne hiers
December 22, 2025 AT 11:01For those asking about GALAD score validation: recent multi-center cohorts (n=3,200) show AUC of 0.87 for HCC detection in post-SVR cirrhotics, outperforming AFP (AUC 0.68). Still not FDA-approved for routine use, but emerging as a promising adjunct. Keep your FIB-4 and FibroScan on file - they’re your baseline.
Edward Stevens
December 22, 2025 AT 11:30So let me get this straight - we cured a virus that took decades to destroy your liver… and now we’re supposed to get ultrasounds forever because your liver still remembers the trauma? Sounds like a really expensive therapy for emotional baggage.
Jonny Moran
December 23, 2025 AT 12:01Edward - you’re not wrong to feel that way. But think of it like this: you survived a war. You don’t stop checking your armor just because the enemy’s gone. Your liver’s still got shrapnel. A simple ultrasound is your check-up. It’s not about fear - it’s about respect for how far you’ve come.
Rich Robertson
December 25, 2025 AT 10:14As someone who lived through the interferon years and then got cured with DAAs - I can tell you this: the relief is real. But the vigilance? That’s the new normal. I’m 62 now. I had F4. I get my scan every six months like clockwork. My wife says I’m obsessive. I say I’m alive. There’s a difference.
Sinéad Griffin
December 26, 2025 AT 04:23USA guidelines are trash. Europe gets it. We need to stop letting Big Pharma dictate liver care. If you’re not screening F3, you’re gambling with lives. And don’t tell me it’s "low risk" - I’ve seen the stats. One missed cancer is one too many. #ScreenEveryF3
Tim Bartik
December 27, 2025 AT 19:39Y’all act like the liver’s some delicate flower. Nah. It’s a goddamn beast. It’s been through hell and still keeps pumping. But yeah - if you got cirrhosis, you ain’t outta the woods. Get the damn scan. Stop being lazy. Your liver didn’t heal because you cried - it healed because your body fought. Now show it some respect.
Natalie Koeber
December 29, 2025 AT 07:31Wait… so they cured HCV but still want you to get ultrasounds? Sounds like the pharma companies just made a new money machine. What if the cancer risk is just fear-mongering? What if they’re hiding that DAAs cause long-term DNA damage? I read a guy on a forum who said his liver enzymes went wild after treatment…
Wade Mercer
December 29, 2025 AT 22:55If you’re not screening after SVR, you’re not just being careless - you’re betraying everyone who fought through interferon, who lost friends to liver failure, who begged for a cure. This isn’t a personal choice. It’s a moral obligation. You got lucky. Don’t waste it.
Sarthak Jain
December 31, 2025 AT 13:19Bro i got svr last year and my fib4 dropped from 4.1 to 2.8… do i still need scan? my doc said maybe not but im scared. any1 else had this?
jeremy carroll
December 31, 2025 AT 22:03Man, I was in the same boat. My fib4 was 3.9 pre-treatment, now it’s 2.5. I asked my hepatologist point blank - "am I safe?" He said "not completely, but your risk is now in the low single digits." We agreed on a scan in 12 months, not 6. It’s not black and white. But don’t skip it.
Daniel Thompson
January 2, 2026 AT 19:50It’s ironic. We celebrate the cure of hepatitis C as a medical triumph, yet we fail to institutionalize the long-term follow-up protocols that make that triumph meaningful. The healthcare system rewards intervention, not continuity. We’ve created a generation of survivors who are left to navigate the aftermath alone - because no one told them the war wasn’t over.