How to Reduce Costs for Specialty Medications and Injectables
 Jan, 17 2026
Jan, 17 2026
Specialty medications and injectables are changing how we treat chronic diseases - but they’re also breaking the bank. These drugs, used for conditions like cancer, rheumatoid arthritis, and multiple sclerosis, make up just 2% of all prescriptions but account for half of all pharmacy spending. A single month’s supply can cost over $1,000. For employers, that’s an average of $34.50 per employee each month - and it’s only getting worse. With spending projected to hit $350 billion by 2027, cutting these costs isn’t optional. It’s urgent.
Start with Formulary Management
One of the most effective ways to control spending is by managing which drugs are covered and under what conditions. This means using formularies - lists of approved medications - to steer patients toward lower-cost, clinically appropriate options. Prior authorization, step therapy, and quantity limits aren’t red tape; they’re tools. For example, Excellus BlueCross BlueShield used prior authorization rules for GLP-1 weight loss drugs and saved $13.64 per member per month compared to national pharmacy benefit managers. That’s not a small number. It adds up fast across thousands of employees. But here’s the catch: if these rules are too strict, patients delay or skip treatment. The key is balance. Use clinical guidelines, not just cost. Involve pharmacists and physicians in the decision-making. A well-run Pharmacy and Therapeutics committee can reduce waste without hurting outcomes.Narrow Your Pharmacy Network
Not all specialty pharmacies are created equal. Some charge more, provide worse support, and have slower turnaround times. By limiting your plan to a small group of high-performing specialty pharmacies, you can cut costs by 10-15%. CarelonRx found that exclusive networks led to lower contract rates and better patient outcomes. One hospital system saved $1.3 billion over three years by switching to a preferred CVS specialty pharmacy network. Why? These networks negotiate bulk pricing, offer dedicated patient coordinators, and track adherence in real time. Patients get faster access to meds, fewer errors, and 24/7 support - all while the plan pays less. The downside? Some members resist switching. Expect a spike in calls during the transition. Solve it with clear communication: send letters, host webinars, and train your HR team to answer questions. Most people will stay once they see the improved service.Switch to Biosimilars When Possible
Biosimilars are the generic version of biologic drugs - complex, injectable medications made from living cells. They’re not copies, but they work the same way. And they cost about half as much. The FDA has approved 42 biosimilars as of late 2023. Yet adoption remains below 30% in most categories. Why? Doctors are hesitant. Patients are wary. Insurance doesn’t always push them. Hospitals that ran structured biosimilar transition programs saw 20-30% cost reductions with no drop in effectiveness. Start by targeting the top 5-10 most expensive biologics in your plan. Work with your PBM to identify biosimilar alternatives. Educate prescribers with data: show them real-world outcomes from other clinics. Offer patient support programs to ease the switch. A patient who was on a $12,000 monthly drug might now pay $6,000 - with the same results.Move Injections Out of Hospitals
Did you know that 91% of specialty drug infusions that happen in hospital outpatient departments could safely be done in a doctor’s office or even at home? A Quantum Health study found that 220 specialty drugs - making up 63% of total spending - were being administered in the most expensive setting possible. Shifting those to a physician’s office or home infusion service cut costs by 48%. A $1,500 hospital infusion became a $780 clinic visit. That’s not magic. It’s basic economics. The trick? Make it easy. Partner with home infusion providers who offer nurse visits, training, and equipment delivery. Build a list of approved outpatient clinics with fair reimbursement rates. Train your staff to ask: “Does this need to be in a hospital?” More often than not, the answer is no.
Use Value-Based Contracts
What if a drug only cost you if it worked? That’s the idea behind value-based contracts. Instead of paying full price upfront, you tie payments to real-world outcomes. Prime Therapeutics reported a 45% year-over-year increase in these arrangements. For example, a cancer drug might come with a guarantee: if the patient doesn’t respond after three months, the manufacturer refunds part of the cost. Or a drug for multiple sclerosis might be priced based on how many relapses the patient has over a year. These contracts are harder to set up. They require data sharing, outcome tracking, and legal agreements. But they’re the future. They shift the risk from the plan to the drugmaker - and that’s where it should be.Maximize Copay Assistance Programs
Manufacturers often offer copay cards to help patients afford expensive drugs. Sounds good, right? But here’s the problem: those cards don’t count toward a patient’s deductible or out-of-pocket maximum. So the patient pays $0 now - but hits their deductible later, when they need other care. Employers using “copay maximizer” programs fix this. These programs replace manufacturer cards with a plan-funded subsidy that counts toward the patient’s out-of-pocket limit. The patient still pays $0 out of pocket - but now, they’re building toward their cap. And the employer saves because they’re not paying for a system that delays cost-sharing. CarelonRx found this approach reduced employer costs by 5-8% annually. It’s ethical, effective, and patient-friendly.Track Data - Relentlessly
You can’t manage what you don’t measure. The best cost-saving programs use real-time analytics to spot outliers early. Who’s getting the most expensive drugs? Are they being used correctly? Is there a pattern of overuse? Quantum Health says successful programs integrate with 3-5 electronic health record and pharmacy systems. That sounds technical, but it’s simple: get alerts when someone starts a $10,000 drug without prior authorization. Flag cases where a patient is on two similar drugs at once. Monitor adherence - if someone stops taking their drug after a month, they’re not saving money; they’re risking hospitalization. Start small. Pick one high-cost drug class. Track usage for six months. Adjust. Repeat.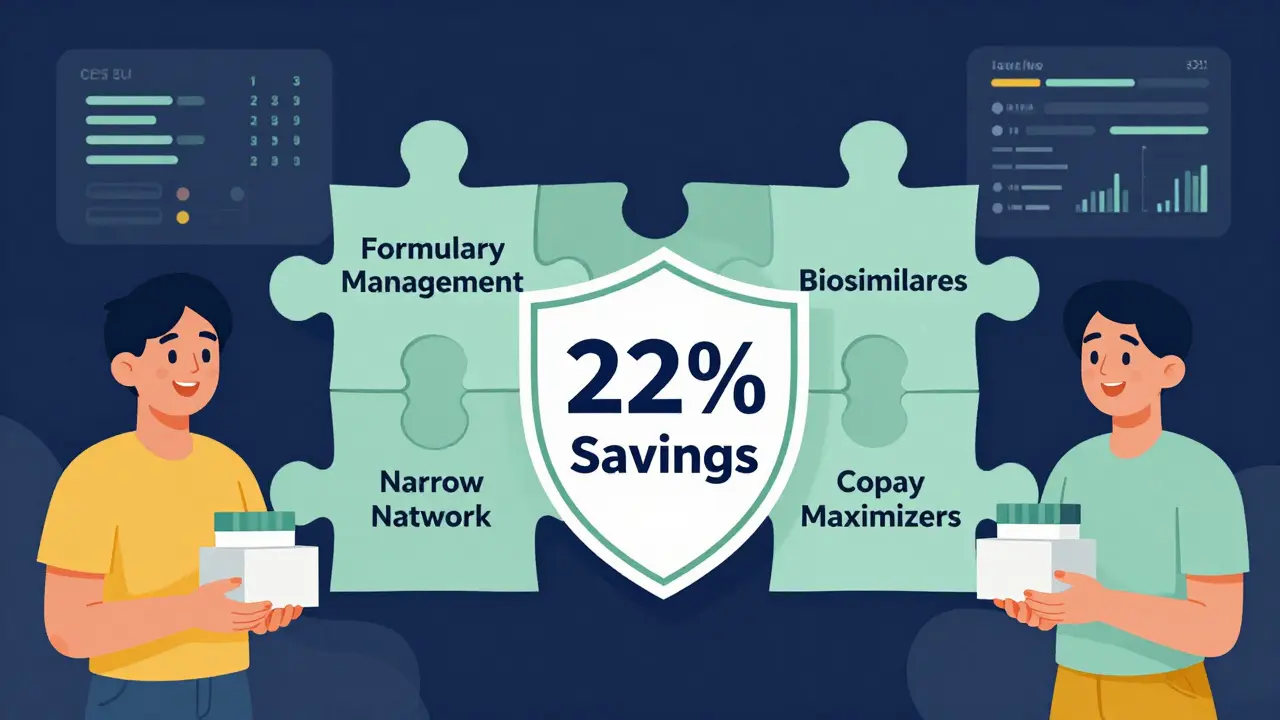
What Doesn’t Work
Some ideas sound smart but fall flat. Capping monthly out-of-pocket costs, for example, makes patients feel better - but doesn’t lower overall spending. It just shifts the cost to the plan. Same with blanket bans on certain drugs. Patients get angry. Clinicians get frustrated. And the problem doesn’t go away. Also avoid switching plans every year. The administrative cost of changing PBM or pharmacy networks often eats up any savings. Stick with a partner for at least three years. Build trust. Refine the system.Real Results, Real People
One large employer with 50,000 employees implemented four strategies: narrow pharmacy network, biosimilar adoption, treatment setting shift, and copay maximizers. In 18 months, they cut specialty drug spending by 22%. That’s $2.4 million saved annually. Patient satisfaction went up. Adherence improved by 14%. No one lost access to care. This isn’t theoretical. It’s happening now.Where to Start
You don’t need to fix everything at once. Pick one area:- If your biggest issue is high drug prices → push for biosimilars.
- If patients are stuck in hospitals for infusions → launch a home infusion program.
- If your PBM isn’t negotiating hard → switch to a network with better contracts.
- If prior authorizations are a mess → hire a dedicated pharmacist to manage them.
Are biosimilars as safe as the original biologic drugs?
Yes. The FDA requires biosimilars to show no clinically meaningful differences in safety, purity, or potency compared to the original biologic. Thousands of patients have used them for years with the same outcomes. In fact, many hospitals now switch new patients to biosimilars by default because they’re just as effective - and half the price.
Why are specialty drugs so expensive?
They’re complex to make, often requiring living cells and strict temperature controls. Development costs are high, and manufacturers have little competition. Many are protected by patents for over a decade. Plus, there’s no universal pricing system - drugmakers set prices based on what the market will bear, not production cost.
Can patients still get their preferred medication if I use a narrow pharmacy network?
Yes, but with conditions. Most networks allow exceptions for medical necessity. If a patient has tried other options and failed, or has an allergy, they can still get the original drug. The goal isn’t to deny care - it’s to encourage smarter, more cost-effective choices first. Clear policies and transparent appeals processes keep patients and providers satisfied.
How long does it take to see savings from these strategies?
Some savings show up in 3-6 months - like shifting infusions to clinics or switching to biosimilars. Others, like formulary changes or value-based contracts, take 12-18 months to fully roll out. Most organizations see a return on investment within 12-18 months. The key is starting early and measuring progress monthly.
What’s the biggest mistake employers make when trying to cut specialty drug costs?
Trying to save money by making it harder for patients to get their meds. Denying access, delaying approvals, or pushing patients to cheaper drugs without clinical support backfires. Patients stop taking their meds. They end up in the ER. Costs go up. The smartest savings come from supporting better care - not restricting it.

Lydia H.
January 17, 2026 AT 22:08Man, I love how this post doesn't just scream 'cut costs!' but actually talks about keeping people healthy while doing it. Too many programs treat patients like line items.
sujit paul
January 18, 2026 AT 12:32One must contemplate the ontological implications of pharmaceutical capitalism: when the cure becomes a commodity, does healing cease to be a moral imperative, or merely a transactional outcome?
Phil Hillson
January 18, 2026 AT 19:34This whole thing is just corporate spin dressed up as compassion
Jackson Doughart
January 19, 2026 AT 20:51I appreciate the data-driven approach here. Shifting infusions from hospitals to clinics isn't just cost-effective-it's clinically logical. The real win is reducing patient stress and travel burden.
Astha Jain
January 20, 2026 AT 01:57biosimilars are just the pharma companies trickin us again lmao
Jake Rudin
January 20, 2026 AT 15:22Let’s be honest: formulary management isn’t about ‘balance’-it’s about who gets to decide what ‘clinically appropriate’ means. Is it the pharmacist? The doctor? The actuary? And who’s accountable when someone’s treatment is delayed because a formulary rule didn’t account for their unique biology? We’re optimizing spreadsheets, not people.
Step therapy sounds reasonable until you’re the one waiting six weeks for a prior auth while your joints turn to cement. And yes, I’ve been there.
It’s not that these strategies are bad-it’s that they’re applied without humility. The system doesn’t care if your pain is real. It only cares if your drug is on the approved list.
And yet-here’s the paradox-we’re told that cost control is moral. But when cost control means denying access, even temporarily, is that morality-or just math with a conscience?
I’ve seen patients cry because they couldn’t afford the co-pay, even with a card. I’ve seen them switch to biosimilars and thrive. I’ve also seen them switch and flare-because biology isn’t a spreadsheet.
So maybe the real innovation isn’t in narrowing networks or shifting infusions-but in designing systems that assume people are complex, not just cost centers.
Can we build a system where the cheapest option isn’t always the first option? Where the patient’s voice isn’t just a footnote in a PBM report?
I’m not against savings. I’m against sanctimony disguised as savings.
If we want to fix this, we need to stop pretending that reducing spending is the same as improving care. It’s not. One is arithmetic. The other is art.
And art takes time. And listening. And sometimes, it costs more.
Malikah Rajap
January 20, 2026 AT 17:27Can we talk about how insane it is that copay cards don’t count toward your deductible? It’s like the system is designed to trick people into thinking they’re saving money, when really they’re just being set up for a bigger financial gut-punch later. I’ve had friends who thought they were getting help-until they hit their deductible and had to pay $8,000 for an MRI because their ‘free’ drug didn’t actually help them reach their out-of-pocket max. This isn’t patient support. It’s financial sleight-of-hand.
And why do we let manufacturers get away with this? They’re not charities-they’re profit-driven. Why should the patient bear the hidden cost of their marketing gimmick? Copay maximizers? Yes. Please. More of this. Let’s stop pretending we’re helping people when we’re just shifting the debt.
Also-why are we still letting drugmakers set prices like they’re auctioning off gold? The R&D costs are real-but so are the billions they make off patents they extend by 37 different loopholes. It’s not capitalism. It’s feudalism with a pharmacy counter.
Aman Kumar
January 21, 2026 AT 21:00Let me decode the corporate lexicon for you: 'formulary management' = rationing under the guise of clinical governance. 'Narrow network' = we're cutting out your preferred pharmacy because they don't kick back enough. 'Biosimilars' = we're forcing you onto a cheaper version because the original is too profitable for the manufacturer to abandon. 'Value-based contracts' = we're outsourcing risk to the patient because the drugmaker won't eat the loss. And 'copay maximizers' = we're pretending we care about your deductible while quietly increasing our own margins. This isn't reform. It's rebranding.
And don't get me started on the 'home infusion' push-because nothing says 'we care about your well-being' like sending a nurse to your living room while your insurer saves $700 per visit. The real cost? Your dignity. Your autonomy. Your right to choose where you receive care.
The only thing that will truly fix this is price regulation. Not 'strategies.' Not 'partnerships.' Not 'data analytics.' Just-regulate the damn prices. They're not expensive because they're complex. They're expensive because they can be.
Lewis Yeaple
January 22, 2026 AT 19:26The data presented is methodologically sound, particularly the 48% reduction in infusion costs via care setting reallocation. However, the omission of Medicare Part B reimbursement dynamics is a significant oversight. In institutional settings, the 6% add-on payment for drugs administered in hospital outpatient departments creates a perverse incentive for providers to favor higher-cost venues. This structural distortion is not addressed in the proposed solutions and must be accounted for in any comprehensive cost-containment strategy.
Furthermore, the assertion that biosimilar adoption rates remain below 30% is misleading without contextualizing prescriber inertia and patient perception biases. A 2022 JAMA study demonstrated that when physicians receive structured education on biosimilar equivalence, adoption increases to 68% within 12 months. The barrier is not clinical uncertainty-it is communication failure.
Value-based contracts, while promising, require interoperable EHR integration and standardized outcome metrics, which remain fragmented across payers. Without federal standardization, scalability is limited. The path forward is not just operational-it is regulatory.
Erwin Kodiat
January 23, 2026 AT 17:37I’ve seen this work firsthand. My cousin switched from the brand-name biologic to a biosimilar for RA-and her flare-ups actually got better because she finally had the money to take it consistently. The old drug cost $14k/month. The new one? $6k. She didn’t feel different. The only difference? She stopped skipping doses because she was terrified of her next bill.
Also-home infusions? Game changer. My mom got her weekly shot in her pajamas with her dog on the bed. No parking, no waiting, no $200 copay for the ‘clinic visit.’ She said it felt like care, not a transaction.
People aren’t against saving money. They’re against being treated like a number. This post gets that.
Valerie DeLoach
January 24, 2026 AT 11:13One of the most thoughtful, human-centered approaches to cost containment I’ve read in years. It’s rare to see a piece that doesn’t sacrifice patient dignity on the altar of efficiency. The emphasis on clinical collaboration, patient education, and systemic transparency-not just cost-cutting-is what makes this actionable and ethical.
Also, thank you for calling out copay cards as a trap. That’s the hidden tax on the sick. We need more copay maximizers. More transparency. More accountability.
And for the record: biosimilars aren’t ‘generic.’ They’re sophisticated, FDA-vetted, clinically equivalent alternatives. The stigma around them is manufactured by fear, not science.
This isn’t just a cost-saving strategy. It’s a model for how healthcare should work: smart, fair, and centered on people.
Tracy Howard
January 25, 2026 AT 03:08Wow. So we’re supposed to be grateful that American corporations are finally getting around to not completely screwing patients? Meanwhile, Canada and the UK have had drug price caps for decades. We’re not ‘innovating’ here-we’re catching up to what other developed nations did 20 years ago.
Also, ‘narrow networks’? That’s just another way of saying ‘we’re cutting your access.’ Don’t dress it up. You’re not saving money-you’re just making patients jump through more hoops so your stock price looks better.
And don’t get me started on biosimilars. The FDA says they’re equivalent. But when the original drug is made in a lab in Switzerland and the biosimilar is made in a factory in India, ‘equivalent’ doesn’t mean ‘identical.’ Don’t fool yourself.
Stop pretending this is about care. It’s about profit. Always has been.
Josh Kenna
January 26, 2026 AT 08:30you know what’s wild? the fact that we’re even having this conversation. like… why is a monthly shot for arthritis costing more than a used car? i’m not mad, i’m just disappointed. also-i think the home infusion thing is genius. my aunt did hers at home and she said it was the first time she didn’t feel like a patient. just a person. that matters.
also-copay cards are a scam. full stop. i didn’t know they didn’t count toward my deductible until i hit it and had to pay $9k for a hospital stay. i was like… wait, i thought i was ‘saving’ money??
anyway-this post is the most useful thing i’ve read all month. thank you. seriously.
Christi Steinbeck
January 28, 2026 AT 00:05As the author of this post, I want to say thank you to everyone who engaged thoughtfully. The pushback on biosimilars? Valid. The anger about copay cards? Necessary. The cynicism about corporate motives? Understandable.
But here’s what I’ve learned in 12 years working in this space: the system isn’t broken because people are greedy-it’s broken because we’ve never built it with patients as the center. We designed it for spreadsheets, not lives.
These strategies aren’t perfect. But they’re a start. And if we keep listening-really listening-to the people who live this every day, we can make it better.
Not cheaper. Better.