How Hypertension Triggers Atrial Fibrillation: What You Need to Know
 Sep, 28 2025
Sep, 28 2025
Quick Take
- High blood pressure strains the heart and can change its rhythm.
- People with hypertension are up to 2‑3 times more likely to develop atrial fibrillation (AF).
- Shared risk factors include age, obesity, sleep apnea, and diabetes.
- Early detection and control of blood pressure dramatically cut stroke risk.
- Lifestyle tweaks and medication work best together.
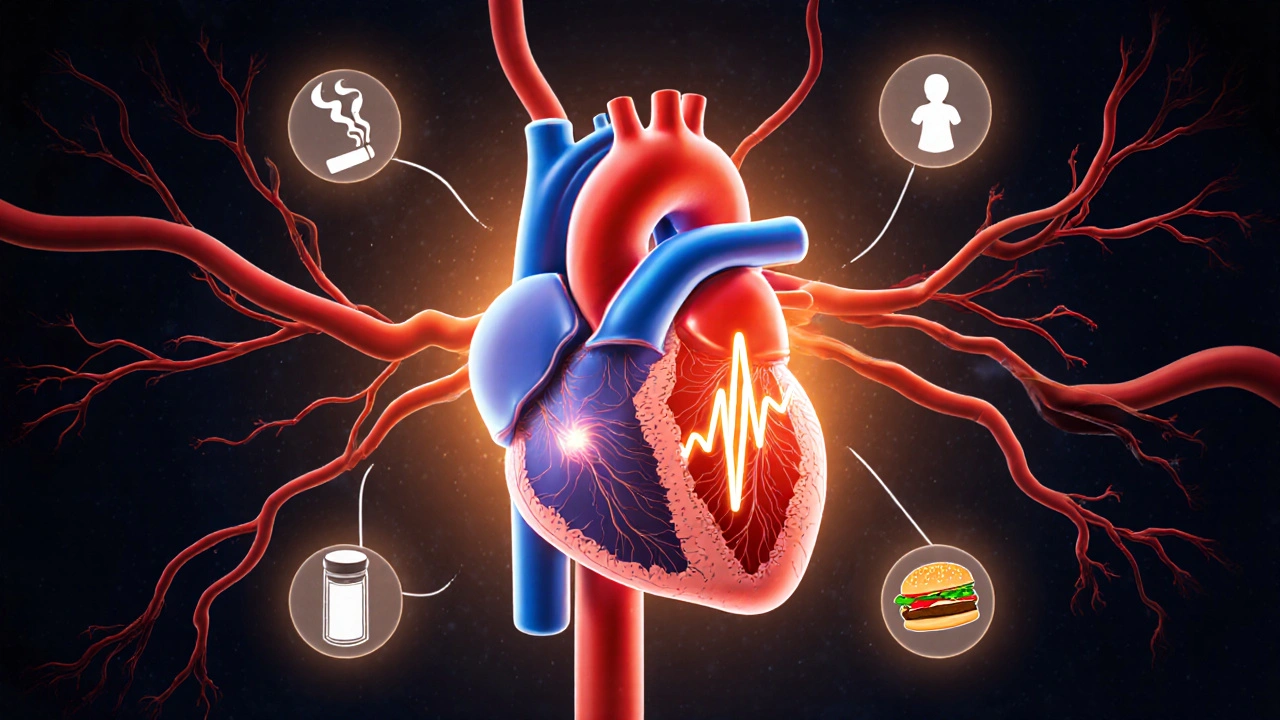
Ever wondered why your doctor keeps talking about blood pressure when you have an irregular heartbeat? The link between hypertension and atrial fibrillation (AF) isn’t just coincidence - it’s a cascade of mechanical stress, electrical remodeling, and shared lifestyle culprits. This guide breaks down the science, the numbers, and the practical steps you can take today.
What Is Hypertension?
Hypertension is a chronic condition characterized by persistently elevated blood pressure, typically defined as a reading of 130/80 mmHg or higher according to the 2023 ACC/AHA guidelines. When the arterial walls are constantly pressurized, they become stiff, and the heart must pump harder to push blood through. Over years, this extra workload can reshape the heart’s chambers, especially the left atrium, setting the stage for rhythm disturbances.
Understanding Atrial Fibrillation
Atrial Fibrillation (AF) is the most common sustained cardiac arrhythmia, where the upper chambers (atria) quiver instead of contracting in a coordinated rhythm. This erratic electrical activity reduces cardiac output and creates a turbulent blood flow that encourages clot formation, raising stroke risk dramatically.
How Elevated Blood Pressure Fuels an Irregular Heartbeat
The relationship isn’t a one‑way street; high pressure triggers several physiological changes that promote AF:
- Left atrial enlargement: The left ventricle works against higher resistance, leading to increased pressure in the left atrium. Over time, the atrial walls stretch, which disrupts the normal electrical pathways.
- Fibrosis and scarring: Chronic stress causes myocardial fibroblasts to deposit collagen, creating scar tissue that acts like electrical roadblocks.
- Neuro‑hormonal activation: Hypertension stimulates the renin‑angiotensin‑aldosterone system (RAAS), which not only raises pressure but also promotes inflammation and electrical remodeling.
Studies from the Framingham Heart cohort (2022) show that every 10‑mmHg rise in systolic pressure adds roughly a 15% increase in AF incidence.
Shared Risk Factors: The Overlap Is Bigger Than You Think
Both conditions thrive on a similar set of lifestyle and health variables. Recognizing them helps you cut the odds on both fronts.
- Age - risk climbs sharply after 65.
- Obesity - excess fat raises blood pressure and strains the heart.
- Sleep apnea - intermittent oxygen drops trigger sympathetic spikes that spike pressure.
- Diabetes - high glucose damages blood vessels and accelerates atrial remodeling.
- Alcohol - binge drinking can provoke “holiday heart” AF episodes.

Clinical Implications: What Your Doctor Looks For
Because the two conditions reinforce each other, guidelines now recommend routine rhythm screening for anyone with uncontrolled hypertension, especially if they’re over 60 or have additional risk factors.
Typical evaluation steps:
- Blood pressure measurement (preferably 24‑hour ambulatory monitoring).
- Electrocardiogram (ECG) to detect AF episodes.
- Pulse‑wave Doppler echocardiogram - Echocardiogram provides images of left atrial size and wall thickness, key predictors of AF.
If AF is confirmed, anticoagulation therapy becomes a priority. The CHA₂DS₂‑VASc score, which includes hypertension as a point, helps decide whether a Anticoagulant like apixaban or warfarin is indicated.
Risk Comparison: Hypertensive vs. Normotensive Populations
| Blood Pressure Category | AF Incidence (%) | Relative Risk |
|---|---|---|
| Normal (<120/80 mmHg) | 1.4 | 1.0 (reference) |
| Elevated (120‑129/<80 mmHg) | 2.1 | 1.5 |
| Stage1 Hypertension (130‑139/80‑89 mmHg) | 3.4 | 2.4 |
| Stage2 Hypertension (≥140/≥90 mmHg) | 5.8 | 4.1 |
The table makes it clear: as pressure climbs, so does the odds of developing AF. This is why aggressive blood‑pressure control saves lives.
Lifestyle Strategies That Hit Both Targets
Here’s a practical checklist that tackles the root causes of both hypertension and AF:
- Salt reduction: Aim for < 2,300mg per day; the DASH diet (rich in fruits, veg, low‑fat dairy) lowers systolic pressure by ~8mmHg on average.
- Regular aerobic exercise: 150minutes of moderate activity weekly can drop systolic pressure by 5‑7mmHg and improve atrial conduction.
- Weight management: Losing 10% of body weight typically reduces pressure by 5mmHg and lessens atrial stretch.
- Limit alcohol: Keep intake below 2 drinks per day; binge episodes raise AF risk fivefold.
- Sleep hygiene: Treat obstructive sleep apnea with CPAP - studies show a 30% reduction in AF recurrence.
- Medication adherence: ACE inhibitors, ARBs, and calcium‑channel blockers not only control pressure but also have anti‑remodeling effects on the atria.
When to Call a Doctor
Don’t wait for a scary episode. Seek medical advice if you notice any of these signs:
- Palpitations, especially a rapid “fluttering” feeling.
- Unexplained fatigue or shortness of breath during everyday activities.
- Sudden dizziness or near‑syncope.
- Consistently high blood pressure readings despite lifestyle tweaks.
Early intervention-whether it’s tweaking meds or starting a home ECG monitor-can prevent strokes and hospitalizations.
Bottom Line
Hypertension isn’t just a number on a cuff; it’s a powerful driver of atrial fibrillation. By recognizing the shared risk factors, staying on top of blood‑pressure goals, and embracing heart‑healthy habits, you dramatically cut the chance of an irregular heartbeat turning into a life‑threatening event.
Frequently Asked Questions
Can I develop atrial fibrillation without having high blood pressure?
Yes. AF can arise from genetics, thyroid disease, heart valve problems, or intense endurance training. However, hypertension remains the single largest modifiable risk factor in the general population.
If I lower my blood pressure, will my atrial fibrillation go away?
Reducing pressure can halt further atrial enlargement and lower the chance of new AF episodes, but existing scar tissue may keep the rhythm abnormal. Many patients need a combination of blood‑pressure meds and rhythm‑control strategies.
What blood‑pressure target should I aim for to protect my heart?
Current guidelines suggest keeping systolic pressure under 130mmHg and diastolic under 80mmHg, especially if you have other risk factors like AF, diabetes, or chronic kidney disease.
Is anticoagulation necessary for everyone with hypertension and AF?
Anticoagulation is guided by the CHA₂DS₂‑VASc score. Hypertension contributes one point, so most patients over 65 will meet the threshold for a blood‑thinner, unless contraindicated.
Can lifestyle changes replace medication for blood‑pressure control?
In early or mild hypertension, diet, exercise, and weight loss can bring readings down enough to avoid drugs. Once blood pressure is consistently high, most clinicians recommend medication plus lifestyle measures for optimal protection.

Grant Wesgate
September 28, 2025 AT 09:47Blood pressure is the silent villain behind many heart rhythm issues.
Richard Phelan
October 1, 2025 AT 10:00Imagine your heart as a disco party and hypertension just cranked the volume to 11.
The walls of your arteries start to sweat, and the atria get confused, stumbling over beats like a drunk dancer.
It's not just hype; the data shows a 15% bump in AF risk for every 10 mmHg rise.
So next time your doc mentions BP, think of it as the DJ you really don’t want.
benjamin malizu
October 4, 2025 AT 10:13Chronic elevation of systolic pressure initiates left atrial stretch, precipitating electrophysiological remodeling via fibroblast‑mediated collagen deposition.
This substrate facilitates re‑entrant circuits, hallmark of atrial fibrillation.
Moreover, neuro‑hormonal activation of the renin‑angiotensin‑aldosterone system compounds ionic current heterogeneity.
Clinically, ambulatory BP monitoring coupled with serial ECGs improves early detection.
Louie Lewis
October 7, 2025 AT 10:27They hide the real connection between blood pressure and heart rhythm the pharma lobby doesn't want you to know.
Mitali Haldankar
October 10, 2025 AT 10:40Interesting take! 😅 Even if it feels like a plot, the science still shows hypertension stresses the atria.
aura green
October 13, 2025 AT 10:53First off, let me say that worrying about blood pressure isn’t just a millennial meme about salads and kale.
Your heart is literally a pump that works overtime when the arteries get stiff, and that overtime adds up like those credit‑card points you never use.
When the left atrium stretches, it’s like trying to fit an oversized pizza box into a tiny fridge-it just doesn't close properly.
That misfit creates little electrical hiccups, which the doctor calls atrial fibrillation, and trust me, those hiccups love to throw a party at night.
Studies from Framingham showed every 10 mmHg bump in systolic pressure adds about a 15 % jump in AF odds, which is basically a statistical slap in the face.
But here’s the good news: you can actually reverse some of that damage with lifestyle tweaks, not just endless meds.
Cutting down on sodium, getting a solid 7‑8 hours of sleep, and shedding a few pounds can shrink that left atrial balloon a bit.
And yes, those boring‑looking CPAP machines for sleep apnea actually keep your oxygen levels steady, which calms the sympathetic nervous system.
If you’re into numbers, the CHA₂DS₂‑VASc score even gives hypertension its own point, reminding you that blood pressure is not a side character.
So, when your physician orders a 24‑hour ambulatory BP monitor, think of it as a reality TV show for your arteries.
Seeing the peaks and valleys lets you target spikes with diet, exercise, or medication before they cause permanent scar tissue.
And don’t forget about the RAAS pathway-ACE inhibitors and ARBs can actually mellow the hormonal fireworks that worsen both pressure and fibrosis.
Bottom line: treat hypertension like you’d treat a leaky roof-fix the source before the ceiling collapses.
Your heart will thank you with smoother beats, fewer episodes of that dreaded ‘holiday heart’ after a few drinks, and a lower stroke risk.
So grab that water bottle, schedule that treadmill session, and keep an eye on those numbers-your atria will survive the drama.
Edward Morrow
October 16, 2025 AT 11:07Look, the moment you ignore your BP numbers you’re basically signing up for a heart‑ache marathon. The government loves the pharma cash flow, so they’ll downplay the simple fixes. Wake up, control that pressure, or keep feeding the AF machine.
Shayne Tremblay
October 19, 2025 AT 11:20Great breakdown! Keeping an eye on blood pressure is like giving your heart a regular tune‑up, and the extra cardio can make a huge difference. Let’s keep sharing these tips and motivate each other to stay on top of both BP and rhythm.
Stephen Richter
October 22, 2025 AT 11:33Indeed, regular monitoring coupled with lifestyle modification yields measurable risk reduction.
Musa Bwanali
October 25, 2025 AT 11:47Don’t let the stats scare you-use them as a battle plan. Hit the gym, cut the salt, and schedule those echo appointments. You’ve got the power to knock AF off the table.
Allison Sprague
October 28, 2025 AT 11:00While the article covers the basics, it could benefit from clarifying the distinction between paroxysmal and persistent AF. Also, a note on the impact of diastolic pressure would round it out.
leo calzoni
October 31, 2025 AT 11:13The elite doctors already know this, but the public keeps missing the point. Hypertension is the root, simple as that.
KaCee Weber
November 3, 2025 AT 11:27Wow, I love how this piece ties together lifestyle factors and hard science 😃. It’s amazing that something as simple as weight loss can shrink the left atrium and lower AF risk. Sleep apnea often flies under the radar, yet fixing it can calm the sympathetic spikes that raise BP. Diabetes adds another layer of inflammation, so managing glucose is a win‑win. And don’t forget the occasional glass of wine-moderation is key, because binge drinking is the real “holiday heart” villain. The CHA₂DS₂‑VASc score is a handy tool; if you’re scoring high, anticoagulation becomes a lifesaver. Bottom line: a holistic approach beats isolated pills every time. Keep sharing these insights, the community thrives on them! 🎉
jess belcher
November 6, 2025 AT 11:40Great info, especially the part about 24‑hour BP monitoring.
Sriram K
November 9, 2025 AT 11:53From a clinical perspective, incorporating ambulatory blood pressure monitoring alongside routine ECGs can catch silent AF early. Educating patients about diet, exercise, and sleep hygiene reinforces the pharmacologic strategy. Feel free to reach out if you need resources on patient education tools.
Maud Pauwels
November 12, 2025 AT 12:07I appreciate the thorough overview. It’s a solid reminder to stay proactive about heart health.