Dupuytren’s Contracture: Causes, Progression, and Proven Treatment Options
 Jan, 23 2026
Jan, 23 2026
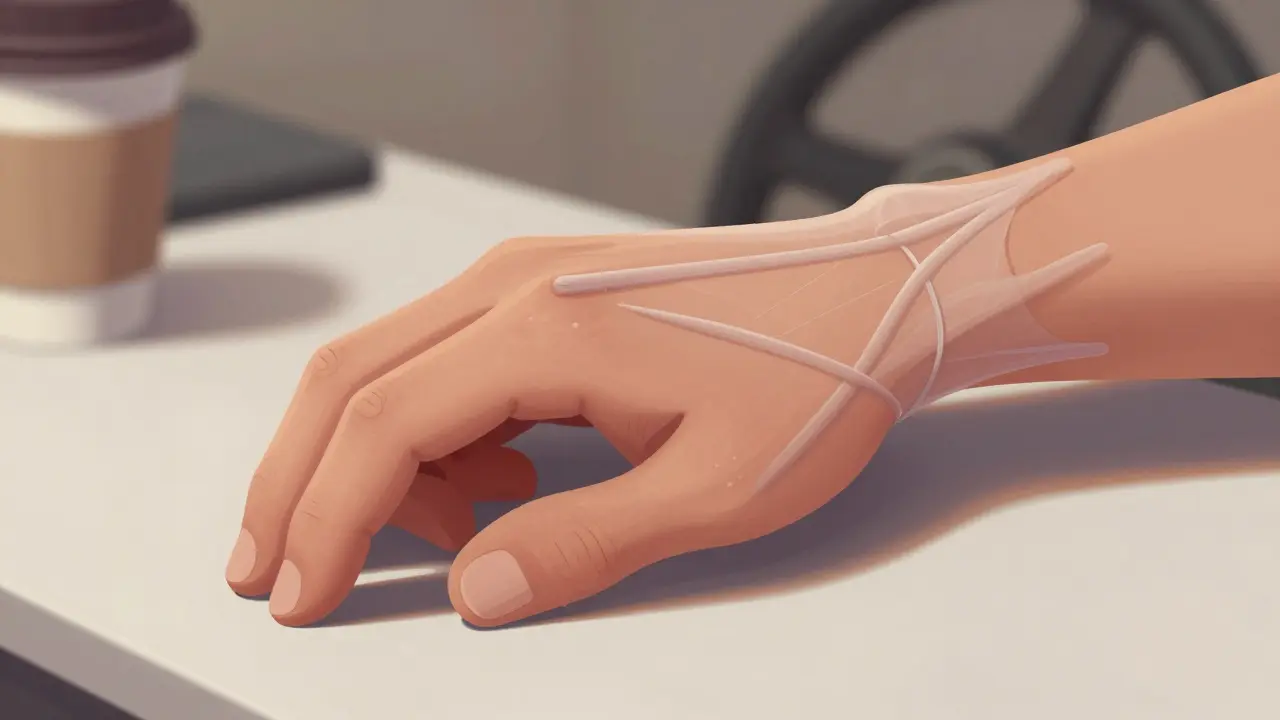
Dupuytren’s contracture isn’t just a bent finger-it’s a slow, silent takeover of your hand’s ability to function. You might notice it first when you can’t lay your palm flat on a table, or when shaking hands feels awkward, like your fingers are stuck in a claw. It doesn’t hurt much at first, which is why so many people ignore it until they can’t grip a steering wheel, hold a coffee cup, or even put their hands in their pockets. By the time it’s obvious, the damage is often advanced. But here’s the truth: you don’t have to wait until it’s too late. Understanding how it starts, how it progresses, and what actually works can change everything.
What’s Really Happening in Your Hand?
Dupuytren’s contracture isn’t arthritis. It’s not a tendon problem. It’s a disease of the palmar fascia-the tough, fibrous layer under your skin that normally holds your hand’s structure in place. In people with this condition, that tissue starts to thicken, tighten, and turn into rope-like cords. These cords pull your fingers-usually the ring and little fingers-down toward your palm. The process is driven by abnormal cells called myofibroblasts that produce too much collagen, the same protein found in scar tissue. These cords can exert more than 10 Newtons of force, enough to permanently bend your joints.
It doesn’t happen overnight. Most people notice small, painless lumps in their palm first-about the size of a pea. These are nodules. Over months or years, they turn into cords that stretch from the palm into the fingers. The progression is unpredictable. Some people stay at Stage 1 for decades. Others go from a lump to a bent finger in under a year. The key trigger? Genetics. If you’re of Northern European descent, especially with family members who’ve had it, your risk jumps from 8% in the general population to nearly 70% if a parent or sibling has it. Age plays a role too. By age 65, up to 30% of people with this ancestry show signs.
How Do You Know It’s Progressing?
There are three simple tests you can do at home to track if it’s getting worse.
- The Table Top Test: Try placing your palm flat on a table. If your fingers don’t lie flat-especially if your ring or little finger lifts up-you’re likely past Stage 2. This test is positive in 92% of people with active cord formation.
- The Dimpling Check: Look closely at your palm. If you see small indentations or puckered skin where the cords are pulling, that’s an early warning. About 68% of patients report this as their first noticeable change.
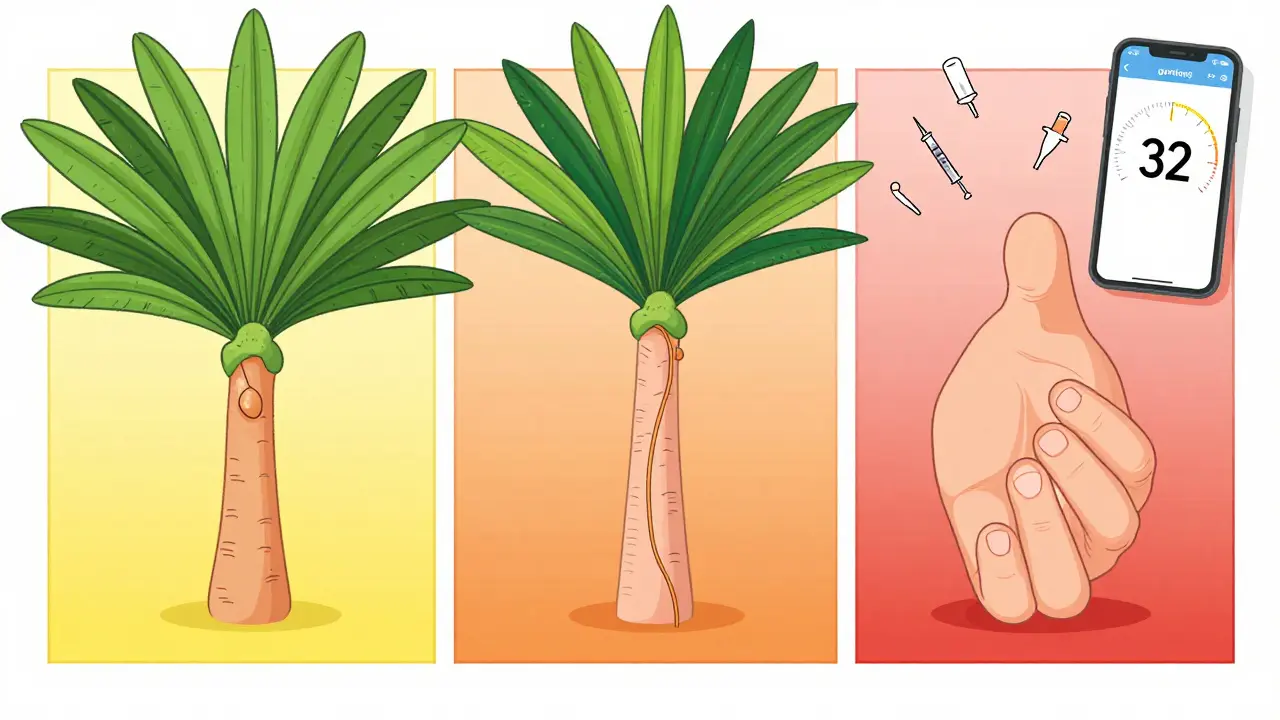
- The Goniometer App: Download a free app like ‘Hand Meter’ on your phone. It uses your camera to measure finger angles. A contracture over 20 degrees at the knuckle (MCP joint) or 30 degrees at the middle joint (PIP joint) is when doctors typically recommend treatment. These apps are 95% accurate compared to clinical tools.
Don’t wait for pain. This condition rarely hurts. But if you can’t open your hand fully, you’re already losing function. The goal isn’t to fix it before it’s bad-it’s to fix it before it stops you from doing what you need to do.
Treatment Options: What Actually Works?
There’s no cure, but there are four proven ways to restore movement. Each has trade-offs in cost, recovery, and risk of recurrence.
Needle Aponeurotomy (NA)
This is the fastest, least invasive option. A doctor uses a needle to poke through the skin and cut the cord under local anesthesia. No stitches. No open surgery. You can straighten your fingers right away. Success rates? 80-90% for early-stage cases. Recovery? Hours, not weeks. Most people go back to work the next day.
But here’s the catch: recurrence is common. In 30-50% of cases, the cord grows back within three years. That’s why it’s best for people who are older, have mild contracture, or aren’t candidates for surgery. It’s also cheaper-$1,500 to $3,000 per hand, compared to $8,000+ for surgery.
Collagenase Injection (Xiaflex)
Xiaflex is an enzyme that dissolves collagen. It’s injected directly into the cord. After 24 hours, your doctor manually straightens your finger. It’s like breaking a rope with chemicals instead of scissors. Success rates are 65-78% for knuckle contractures. It’s FDA-approved and avoids surgery.
But it’s expensive-$3,500 to $5,000 per injection. And it’s not a one-time fix. You might need up to three injections per cord. The big downside? Pain. About 70% of patients report moderate to severe pain during the finger straightening. Skin tears and nerve bruising happen in 5-10% of cases. Still, for people who want to avoid surgery, it’s a solid middle ground.
Open Fasciectomy
This is the classic surgery. The surgeon cuts open the palm and removes the diseased tissue. It’s the most effective long-term solution. Immediate correction is 90-95%. Recurrence? Only 20-30% at five years. It’s the go-to for younger, active people with severe contracture.
But the recovery is brutal. You’ll need 6-12 weeks of physical therapy. Swelling, stiffness, and numbness are common. Nerve injury happens in 3-5% of cases. And the scar? It’s permanent. Still, if you’re a carpenter, a musician, or someone who relies on full hand function, this is often the best bet.
Dermofasciectomy
This is fasciectomy plus skin removal. The surgeon takes out both the diseased fascia and the overlying skin, then replaces it with a skin graft. Why? Because the skin over the cords is often thickened and scarred too. This reduces recurrence to just 10-15% at five years-the lowest of any method.
The trade-off? Recovery takes 3-6 months. You’ll need a skin graft donor site, usually from the forearm or thigh. It’s not for everyone, but for people with recurrent Dupuytren’s or very advanced disease, it’s often the only way to get lasting results.
What Doesn’t Work (And Why)
There are a lot of products out there promising relief: stretching gloves, vitamin E creams, ultrasound devices, even herbal supplements. Most are useless.
Corticosteroid injections? They might reduce pain in the early nodule stage, but they don’t stop cord formation. Studies show only a 30% response rate, and they can weaken the skin over time.
Stretching gloves? They’re marketed as a way to slowly pull fingers straight. But a 2023 survey of 1,542 users found 28% reported skin breakdown, blisters, or no improvement after six months. They’re not harmful, but they’re not a treatment.
And don’t fall for ‘miracle cures’ online. There’s zero evidence that turmeric, bromelain, or acupuncture change the course of this disease. The science is clear: only four methods work-and they’re all mechanical or chemical interventions targeting the cord itself.
Recovery Is Half the Battle
No matter which treatment you choose, recovery is where most people fail. A study from Ohio State found patients who did 80% or more of their prescribed physical therapy regained 95% of their finger motion. Those who skipped sessions? Only 75% recovery.
After surgery or injection, you’ll need to stretch your fingers 4-6 times a day for 5-10 minutes each time. That’s non-negotiable. Most people stick with it for the first month. By month three, adherence drops to 45%. That’s why recurrence happens.
Use a timer. Set phone reminders. Write it down. If you’re serious about keeping your hand functional, this is the work you have to do.

When to See a Specialist
You don’t need to wait until your fingers are bent at 90 degrees. If you can’t do the table top test, or if your fingers are stiff and won’t straighten fully after waking up, it’s time to see a hand specialist. Early intervention doesn’t mean surgery-it means monitoring. Some people never need treatment. But if you’re a manual laborer, a musician, or someone who uses their hands daily, waiting too long can mean permanent loss of function.
Doctors typically recommend treatment when contracture hits 30 degrees at the knuckle or 20 degrees at the middle joint. That’s the threshold where daily tasks start to become difficult. If you’re over 50, have a family history, or notice rapid changes, don’t delay.
What’s Coming Next?
Research is moving fast. Gene therapy targeting the TGF-β1 protein-which drives collagen overproduction-is in early trials. One study showed a 40% reduction in cord thickness after six months. A new device called the Fasciotome, cleared by the FDA in March 2023, uses ultrasound guidance to cut cords with a tiny needle in under 12 minutes-faster than traditional needle aponeurotomy.
Stem cell therapy is also being tested. Early results from the University of Pittsburgh suggest adipose-derived stem cells can reduce recurrence by 55% over two years. These aren’t available yet, but they’re on the horizon.
For now, stick with what works. The tools are here. The data is clear. The choice isn’t between doing nothing and major surgery-it’s between timing, technique, and commitment.
Real Stories, Real Outcomes
One man, a guitarist named ‘GuitarGuy42’ on the ASSH forum, had his ring finger stuck at 60 degrees. He had needle aponeurotomy. Within 48 hours, he was playing again. No rehab. No downtime.
Another, ‘PalmProblem89’, used Xiaflex. His fingers straightened, but the pain during the procedure was so bad he cried. Still, he said he’d do it again-he could finally shake hands without embarrassment.
And then there’s the man who waited five years. He thought it was just aging. By the time he saw a doctor, he couldn’t hold a fork. He had a full fasciectomy. It took eight months to recover. He lost his job as a mechanic. He regrets the delay.
This isn’t a condition you can ignore. It doesn’t go away. But with the right knowledge, you don’t have to lose your hand to it.
Can Dupuytren’s contracture go away on its own?
No. Dupuytren’s contracture is progressive. Once cords form and pull the fingers down, they won’t reverse without medical intervention. Nodules may stop growing, but the cords don’t dissolve. Ignoring it leads to permanent stiffness.
Is Dupuytren’s contracture painful?
Usually not. Early nodules might feel tender for a few months, but once cords form, pain is rare. The main issue is loss of function, not discomfort. If you’re in pain, it could be another condition like arthritis or nerve compression-see a specialist.
Can I prevent Dupuytren’s contracture?
No. There’s no proven way to prevent it. Smoking, alcohol, and diabetes may increase risk, but even healthy people with Northern European ancestry get it. The main risk factor is genetics. You can’t change your genes, but you can monitor your hands and act early if you notice changes.
Which treatment has the lowest recurrence rate?
Dermofasciectomy has the lowest recurrence-only 10-15% at five years. Open fasciectomy follows at 20-30%. Needle aponeurotomy and collagenase have higher recurrence rates, around 30-50% within three years. But recurrence doesn’t always mean you need another procedure-it depends on how much it affects your daily life.
How do I know if I’m a candidate for collagenase injection?
You’re a good candidate if your contracture is at the knuckle (MCP joint), not the middle joint (PIP), and if you’re not a good surgical candidate due to age or health. You must be willing to do the finger extension maneuvers 24 hours after injection. If you’re afraid of pain or can’t commit to the follow-up, needle aponeurotomy may be better.
Will insurance cover Dupuytren’s treatment?
Yes. Most insurance plans cover needle aponeurotomy, collagenase injections, and surgery because they’re medically necessary for restoring hand function. Cosmetic concerns aren’t covered, but functional loss is. Always check your plan’s pre-authorization rules-some require physical therapy trials first.

Shelby Marcel
January 24, 2026 AT 12:00so i just noticed this lump on my palm last week and i was like lol probably nothing right? then i tried the table top test and my ring finger just lifted off like it had a mind of its own. now i’m googling at 2am like a panicked person. anyone else have this happen outta nowhere?
Tiffany Wagner
January 25, 2026 AT 22:12i’ve had this for years. never hurt. just annoying when i can’t high five properly. got needle aponeurotomy last year. back to normal in 2 days. no big deal.
Chloe Hadland
January 25, 2026 AT 22:48thank you for writing this. i’ve been scared to look up what’s happening to my hand because i didn’t want to panic. this felt like someone finally explained it without making me feel crazy.
Amelia Williams
January 26, 2026 AT 21:33just got my Xiaflex shot last week. the pain during the straightening? yeah. it was like someone took a crowbar to my finger and twisted. cried like a baby. but now i can hold my coffee again. worth every second of agony. also, i did the stretching like they said. no recurrance yet. you gotta do the work.
Patrick Gornik
January 27, 2026 AT 12:12let’s be real-this whole thing is a capitalist racket disguised as medicine. the fascia doesn’t ‘contracture’-it’s your body’s way of saying you’ve been living in a silicone-walled dystopia of ergonomic lies. the real cause? overuse of smartphones and the psychological repression of manual labor in post-industrial societies. your body is trying to communicate, but the orthopedic-industrial complex sells you needles and enzymes because they can’t monetize existential awareness. and don’t get me started on how dermatofasciectomy is just the medical-industrial complex’s way of saying ‘we don’t know what we’re doing but we can cut more stuff.’
Meanwhile, your grandma in Norway who worked the loom till she was 80 never had this. Coincidence? Or is your wrist just too soft?
Also, collagenase? That’s just snake oil with a patent. They injected a protein that eats collagen… into your hand. So what happens when it eats your tendons? Or your nerves? Or your soul? You don’t know. But the FDA says it’s fine. Trust the system.
And don’t even get me started on the ‘recovery’ cult. Stretching 4 times a day? That’s not rehab-it’s behavioral conditioning. You’re being trained to be a compliant patient. The real cure? Stop using your hands. Go live in a cabin. Chop wood. Let your fascia breathe. But of course, that’s not profitable.
So yeah. I’m not getting the shot. I’m just gonna let my fingers curl into fists and stare at the sky. Maybe my hand is trying to tell me something deeper than ‘you can’t grip a coffee cup.’ Maybe it’s telling me the whole damn system is broken.
Viola Li
January 27, 2026 AT 21:34you people are so gullible. needle aponeurotomy? collagenase? please. you’re all just feeding the medical machine. i’ve had this since i was 45 and i didn’t do anything. now i’m 68 and my fingers are curled like claws-but i’m happy. i don’t need to ‘grip a steering wheel.’ i drive a tractor. my hands are fine. you’re all obsessed with ‘function’ like your hands are some kind of machine that needs to be calibrated. nature doesn’t care if you can shake hands. your ego does.
Dolores Rider
January 28, 2026 AT 05:40ok but have you heard about the 5G towers? they’re triggering the myofibroblasts. i read it on a forum. my cousin’s neighbor’s dog had this and the vet said it was ‘electromagnetic stress.’ also, glyphosate. it’s in your coffee. and your yoga mats. they want you to think it’s genetic but it’s not. it’s the chemtrails. and the implants. i’m not even gonna say it out loud.
also, i tried the goniometer app and it said i had 32 degrees. so i went to the ER and they gave me a 1000mg dose of vitamin D. now i’m better. it was the fluoride.
blackbelt security
January 29, 2026 AT 22:27you’re not alone. i’ve been there. the table test freaked me out too. but i did the needle thing and now i’m back to lifting weights. it’s not the end of the world. you just have to act before it owns you.
Sushrita Chakraborty
January 31, 2026 AT 03:20Thank you for the detailed, scientifically grounded exposition. I am from India, and while Dupuytren’s is less prevalent here, I have observed similar fascial abnormalities in elderly patients with a history of manual labor. The distinction between fibrosis and degenerative arthritis is often blurred in primary care settings. Your emphasis on early detection through objective metrics-such as the goniometer app-is commendable. I shall share this with my colleagues in Mumbai.
Sharon Biggins
January 31, 2026 AT 13:02just wanted to say you’re doing great. i’ve been there too. the stretching feels pointless sometimes but i do it anyway. one day at a time. you got this.
John McGuirk
January 31, 2026 AT 18:07they’re lying about the recurrence rates. the real numbers are hidden. i know a guy who had the surgery. three months later, his hand swelled up and they said ‘oh it’s just inflammation.’ but he saw the cord growing back. they don’t tell you that. they just bill you again. it’s all a loop. they want you hooked. like a drug.
Vatsal Patel
February 2, 2026 AT 17:47ah yes, the classic ‘science’ narrative. let me guess-you also believe in ‘vaccines’ and ‘climate change’? Dupuytren’s is just your body rejecting modernity. your hands were meant to grip rope, not touchscreens. you’re not sick-you’re out of sync. the solution isn’t surgery. it’s meditation. and maybe a return to barefoot living.
Also, ‘FDA-approved’? That’s just a fancy stamp for ‘we got paid.’
Tommy Sandri
February 2, 2026 AT 18:11It is noteworthy that the prevalence of Dupuytren’s contracture in populations of Northern European descent aligns with historical genetic drift patterns observed in the Viking expansion. The condition’s association with fibroblast dysregulation is well-documented in peer-reviewed literature, and the treatment modalities referenced represent the current standard of care as endorsed by the American Society for Surgery of the Hand. While cultural perceptions of hand function vary, clinical outcomes remain consistent across socioeconomic strata when early intervention is pursued.
asa MNG
February 4, 2026 AT 08:19OMG I JUST REALIZED MY DAD HAD THIS AND HE NEVER TOLD ME 😭😭😭 I’M GONNA DIE AND MY HANDS WILL BE CLAWS AND NO ONE WILL LOVE ME 😭😭😭 I’M 28 AND I JUST TRIED THE TABLE TEST AND MY PINKY IS LIKE 15 DEGREES UP 😭 I NEED TO SEE A DOCTOR TOMORROW I’M SO SCARED 😭😭😭