Digoxin and Amiodarone: How to Prevent Deadly Drug Interactions
 Dec, 8 2025
Dec, 8 2025
Digoxin-Amiodarone Interaction Calculator
Important Safety Information
This tool helps determine the appropriate digoxin dose adjustment when starting amiodarone. Without adjustment, digoxin levels can double, risking toxicity. Always consult with a healthcare provider before making any medication changes.
When two powerful heart drugs are mixed, the consequences can be deadly - and it’s not always obvious when it’s happening. Digoxin and amiodarone are both used to treat irregular heart rhythms, but together, they can push digoxin levels into toxic territory. This isn’t a rare mistake. It’s a well-known, preventable crisis that still happens in hospitals and clinics across the country - especially in older patients with kidney problems.
Why This Interaction Is So Dangerous
Digoxin has one of the narrowest therapeutic windows in all of medicine. The difference between a therapeutic dose and a toxic one is tiny: 0.5 to 0.9 ng/mL. Go just a little above that, and you risk nausea, vomiting, blurry yellow vision, confusion, and dangerous heart rhythms like bradycardia or ventricular tachycardia. Amiodarone, on the other hand, is a potent antiarrhythmic with a half-life of up to 100 days. That means once it’s in your system, it stays there - for months. The problem isn’t just that amiodarone increases digoxin levels. It’s how much and how long. Studies show that when amiodarone is started, digoxin blood levels can jump by 100% or more. That’s not a small fluctuation - that’s a leap from safe to life-threatening. In one landmark study from 1984, patients on digoxin who started amiodarone saw their digoxin levels rise from an average of 0.97 ng/mL to nearly 2.0 ng/mL. That’s double the upper limit of safety.How It Happens: The Science Behind the Risk
Amiodarone doesn’t just interact with digoxin - it hijacks how your body clears it. Digoxin is normally removed from your body through two main paths: your kidneys and a transporter protein called P-glycoprotein in your gut and liver. Amiodarone blocks that transporter. Think of P-glycoprotein as a gatekeeper that pushes digoxin out of your cells. When amiodarone shuts it down, digoxin builds up inside your bloodstream. Research from 2023 confirms that this P-glycoprotein inhibition accounts for 60-70% of the interaction. Amiodarone also slightly slows down how fast your liver breaks down digoxin. The result? Digoxin lingers. And because amiodarone sticks around for so long, the danger doesn’t disappear after a few days. It lingers for weeks - even after you stop taking amiodarone.Who’s Most at Risk?
This isn’t a risk for everyone. It’s concentrated in specific groups:- Patients over 70 years old
- Those with chronic kidney disease (eGFR under 60 mL/min)
- People on long-term digoxin for heart failure or atrial fibrillation
- Patients already on low digoxin doses (0.125 mg daily) - because even a small increase pushes them into toxicity
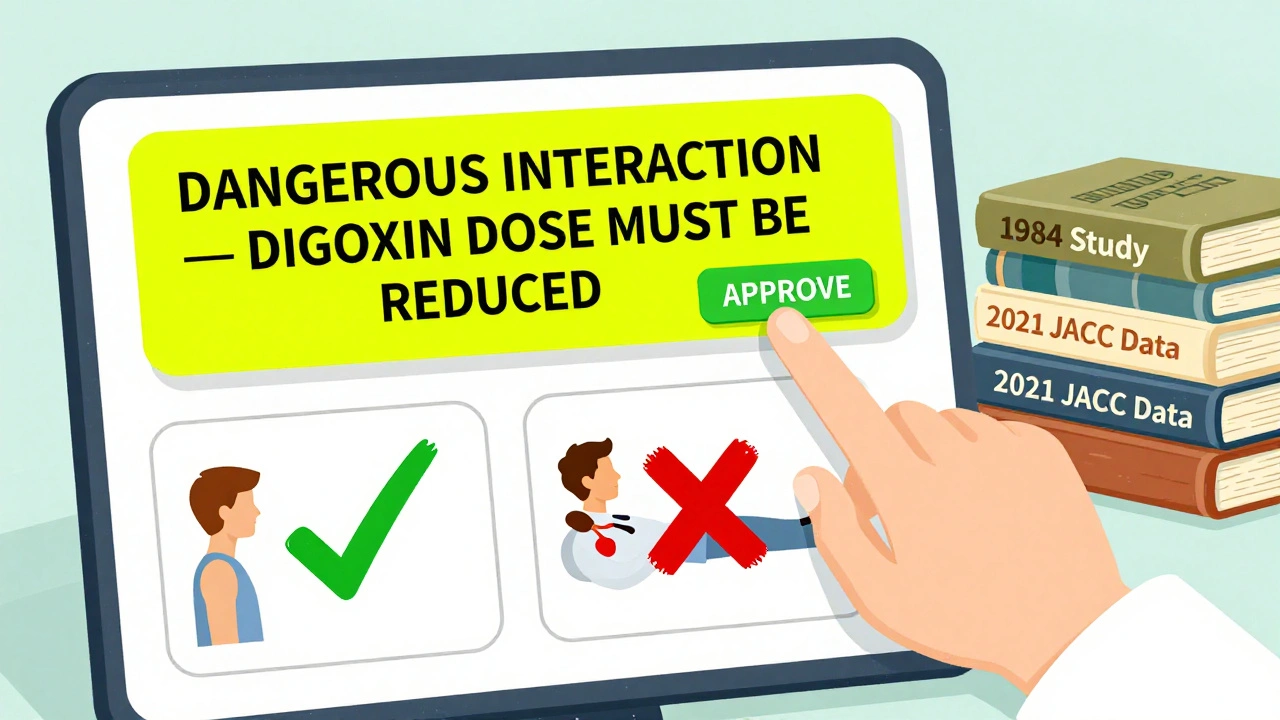
What Doctors Should Do - And Often Don’t
Guidelines have been clear for decades. The European Heart Rhythm Association, the American Heart Association, and the American Society of Health-System Pharmacists all agree: when you start amiodarone in a patient taking digoxin, cut the digoxin dose in half - immediately. But here’s the problem: only about 44% of hospitals actually do it. A 2022 study across 15 U.S. academic centers found that in community hospitals, the error rate jumped to 68%. Why? Because the interaction isn’t always on the radar. Amiodarone is often prescribed for acute arrhythmias, and digoxin is seen as a routine, harmless maintenance drug. Clinicians forget to check. Or they assume the patient’s current digoxin level is fine - not realizing that levels can rise slowly over days or weeks. One case from Massachusetts General Hospital involved a 72-year-old woman with atrial fibrillation. She was started on amiodarone for a fast heart rate and kept on her usual 0.25 mg digoxin daily. Within five days, she developed severe bradycardia and hyperkalemia (potassium levels hit 6.8 mEq/L - dangerously high). She ended up in the ICU for four days. Her digoxin level? 3.1 ng/mL. Toxic.
The Right Way to Manage It
There’s a clear, step-by-step protocol that works - and it’s simple:- Check the patient’s digoxin level before starting amiodarone. Don’t assume it’s fine.
- Reduce the digoxin dose by 50% the day you start amiodarone - no waiting, no exceptions.
- Recheck the digoxin level 72 hours after starting amiodarone. If it’s still above 0.9 ng/mL, reduce further.
- For patients with kidney impairment (eGFR under 50 mL/min), reduce digoxin by 67% (to one-third of the original dose).
- Continue monitoring levels weekly for the first month. The peak interaction can take 1-2 weeks to show up.
What About Stopping Amiodarone?
Here’s where many get caught off guard. Amiodarone doesn’t leave your system quickly. Even after you stop taking it, its active metabolite, desethylamiodarone, sticks around for up to 60 days. That means the interaction doesn’t vanish just because the drug is discontinued. If a patient stops amiodarone, don’t automatically increase the digoxin dose back to original levels. Wait. Monitor. Recheck levels after 2-4 weeks. Only then, if levels are low and the patient still needs digoxin, consider a slow, cautious increase.Why This Interaction Is Still Happening
Despite decades of evidence, this interaction persists because of three things:- Complacency - “Digoxin’s been used for 70 years, it’s safe.”
- Fragmented care - A cardiologist prescribes amiodarone, a primary care doctor manages digoxin, and no one talks.
- Lack of alerts - Many electronic health records still don’t flag this combo as high-risk.
The Bigger Picture: Is Digoxin Still Worth It?
The rise of safer alternatives like beta-blockers and calcium channel blockers has made digoxin less popular. Since 2010, its use in atrial fibrillation has dropped by 32%. But it hasn’t disappeared. For patients with heart failure and atrial fibrillation who can’t tolerate other drugs, digoxin still has a role. The 2024 European Society of Cardiology guidelines now recommend avoiding digoxin altogether if amiodarone is planned. That’s the safest path. But if digoxin is already being used - and you need to add amiodarone - you don’t have a choice but to manage the interaction properly.What Patients Should Know
If you’re taking digoxin and your doctor says you need amiodarone, ask:- “Will my digoxin dose be changed?”
- “When will my blood level be checked again?”
- “What symptoms should I watch for - nausea, dizziness, seeing halos around lights?”
What’s Next?
The DIG-AMIO trial, currently underway, is comparing 50% vs. 33% digoxin dose reductions when starting amiodarone. Results are expected in late 2025. But we don’t need to wait. The evidence right now is overwhelming: cut the dose. Monitor closely. Save lives.Can I take digoxin and amiodarone together safely?
Yes - but only if the digoxin dose is reduced by at least 50% at the time amiodarone is started. Without this adjustment, the risk of life-threatening digoxin toxicity is very high. Never take both drugs at full doses together.
How long does the digoxin-amiodarone interaction last?
The interaction can last for months. Amiodarone has a half-life of up to 100 days, and its active metabolite stays in the body for up to 60 days after stopping. Even after you stop amiodarone, digoxin levels may remain elevated. Always monitor levels for at least 2-3 months after discontinuation.
What are the signs of digoxin toxicity?
Symptoms include nausea, vomiting, loss of appetite, confusion, visual changes (like yellow or green halos around lights), slow or irregular heartbeat, dizziness, and fainting. High potassium levels may also occur. If you experience any of these while taking both drugs, seek medical help immediately.
Should I stop digoxin if I need amiodarone?
Not necessarily. If digoxin is needed for heart failure control, reducing the dose by 50% (or 67% if kidney function is poor) is the standard approach. Stopping digoxin entirely may worsen heart failure symptoms. The goal is to keep digoxin at a safe level, not to eliminate it.
Is this interaction only a problem in older adults?
No - but older adults and those with kidney disease are at much higher risk. Younger, healthy patients with normal kidney function may tolerate the interaction better, but they are still at risk. The interaction affects everyone taking both drugs - the degree of risk just varies.
Can other drugs cause the same interaction?
Yes - other drugs that inhibit P-glycoprotein, like verapamil, quinidine, and some antibiotics (clarithromycin, erythromycin), can also raise digoxin levels. But none are as potent or as long-lasting as amiodarone. Amiodarone remains the most dangerous and clinically significant interaction with digoxin.

Rich Paul
December 9, 2025 AT 13:59yo so digoxin and amiodarone together is basically a russian roulette pill combo? i had an old lady in my unit last month who started seeing yellow halos and thought she was in a disco. turned out her digoxin was at 3.2. doc didn’t cut the dose. she ended up in the icu for a week. smh.
Katherine Rodgers
December 10, 2025 AT 09:22lol at the 44% of hospitals that actually follow guidelines. guess that’s why we’re all just one missed lab result away from a funeral. i swear if i see one more ‘digoxin is harmless’ comment i’m gonna scream. it’s not 1950 anymore, people.
Mona Schmidt
December 12, 2025 AT 07:38Thank you for this comprehensive breakdown. The P-glycoprotein mechanism is often glossed over in clinical teaching, yet it’s the cornerstone of this interaction. I’ve seen residents assume that because a patient’s digoxin level was ‘normal’ at admission, no adjustment is needed - unaware that amiodarone’s delayed onset means toxicity can emerge days later. This isn’t just about dosing - it’s about vigilance. I now include a checklist in my handoffs: 1) Confirm digoxin dose reduction at amiodarone initiation, 2) Schedule level check at 72 hours, 3) Flag renal impairment as a multiplier risk. Small systems, big impact.
Ronald Ezamaru
December 12, 2025 AT 11:31As someone who’s worked in rural ERs for 18 years, this is the kind of thing that keeps me up at night. We don’t always have pharmacists on site. We don’t always have EHR alerts. We just have a chart, a calculator, and a gut feeling. That’s why guidelines matter - not as bureaucracy, but as lifelines. I’ve lost two patients to this interaction. Both were on 0.125 mg digoxin. Both were told ‘it’s fine.’ Neither made it out of the hospital.
Lola Bchoudi
December 14, 2025 AT 03:51Let’s not forget the elephant in the room: digoxin is still used because it’s cheap. In a system where cost trumps safety, this interaction thrives. I’ve seen patients on Medicare get amiodarone prescribed because it’s covered, while safer alternatives are denied due to prior auth. Then they’re told to ‘just cut the digoxin in half’ - but no one helps them navigate the pharmacy, the lab, or the follow-up. It’s not just a pharmacokinetic problem - it’s a structural failure.
Christian Landry
December 15, 2025 AT 14:52just had a patient on this combo last week - doc didn’t adjust the digoxin. i was like ‘uhhh…’ and pulled up the 2023 paper on p-gp inhibition. turned out his level was 2.8. he was confused and had a 42 bpm heart rate. we dropped the digoxin to 0.0625 mg and rechecked in 72 hrs. down to 0.7. saved him. also, side note: amiodarone’s half-life is wild. my grandma’s still got traces of it in her system 8 months after she stopped it. 🤯
Morgan Tait
December 17, 2025 AT 03:51you know what’s really happening? Big Pharma doesn’t want you to know this. Digoxin is old, cheap, and generic. Amiodarone? Patent-protected, expensive. If everyone knew how dangerous this combo is, hospitals would stop prescribing amiodarone altogether. But they won’t - because the profit margins on amiodarone are too good. The ‘guidelines’? Just noise. The real solution? Ban amiodarone. Or better yet - ban all drugs with half-lives longer than your attention span.
Darcie Streeter-Oxland
December 17, 2025 AT 07:50It is regrettable that the manuscript, whilst meticulously detailed, fails to adequately address the medicolegal implications of non-adherence to established clinical protocols. One must question whether the cited institutional outcomes are attributable solely to dose reduction, or whether confounding variables - such as documentation practices, nurse-to-patient ratios, or compliance with monitoring schedules - were sufficiently controlled. A robust multivariate analysis is conspicuously absent.