CYP450 Enzyme Interactions: How Medications Compete for Metabolism
 Feb, 13 2026
Feb, 13 2026
Imagine taking your usual blood pressure pill and a new antibiotic, only to find out your body can’t process either one properly. That’s not a hypothetical scenario-it happens every day because of something called CYP450 enzyme interactions. These enzymes don’t just break down drugs; they’re like a crowded subway turnstile where every pill tries to get through at once. And when too many drugs push in at the same time, some get stuck-leading to dangerous side effects or treatment failure.
What Exactly Are CYP450 Enzymes?
CYP450 enzymes are a family of proteins in your liver and intestines that handle about 90% of all prescription medications. Think of them as your body’s main drug-deactivation team. They don’t just remove drugs-they sometimes activate them. For example, codeine needs CYP2D6 to turn into morphine to work as a painkiller. If CYP2D6 is blocked, the codeine does nothing. If it’s overactive, you get too much morphine-and that’s dangerous.
There are six major CYP450 enzymes doing most of the work:
- CYP3A4: Handles half of all medications, including statins, blood thinners, and opioids.
- CYP2D6: Manages 25% of drugs, especially antidepressants, beta-blockers, and pain meds like codeine.
- CYP2C9: Breaks down warfarin (a blood thinner), NSAIDs, and some diabetes drugs.
- CYP2C19: Important for clopidogrel (Plavix), proton pump inhibitors, and some antidepressants.
- CYP1A2: Metabolizes caffeine, theophylline, and certain antipsychotics.
- CYP2E1: Deals with alcohol, acetaminophen, and some anesthetics.
These enzymes are not just passive cleaners-they’re competitive. Each one has a limited number of slots. When Drug A and Drug B both need CYP3A4, they fight for space. The stronger binder wins. That’s why grapefruit juice can be dangerous: it blocks CYP3A4 in your gut, causing drugs like simvastatin to build up to toxic levels.
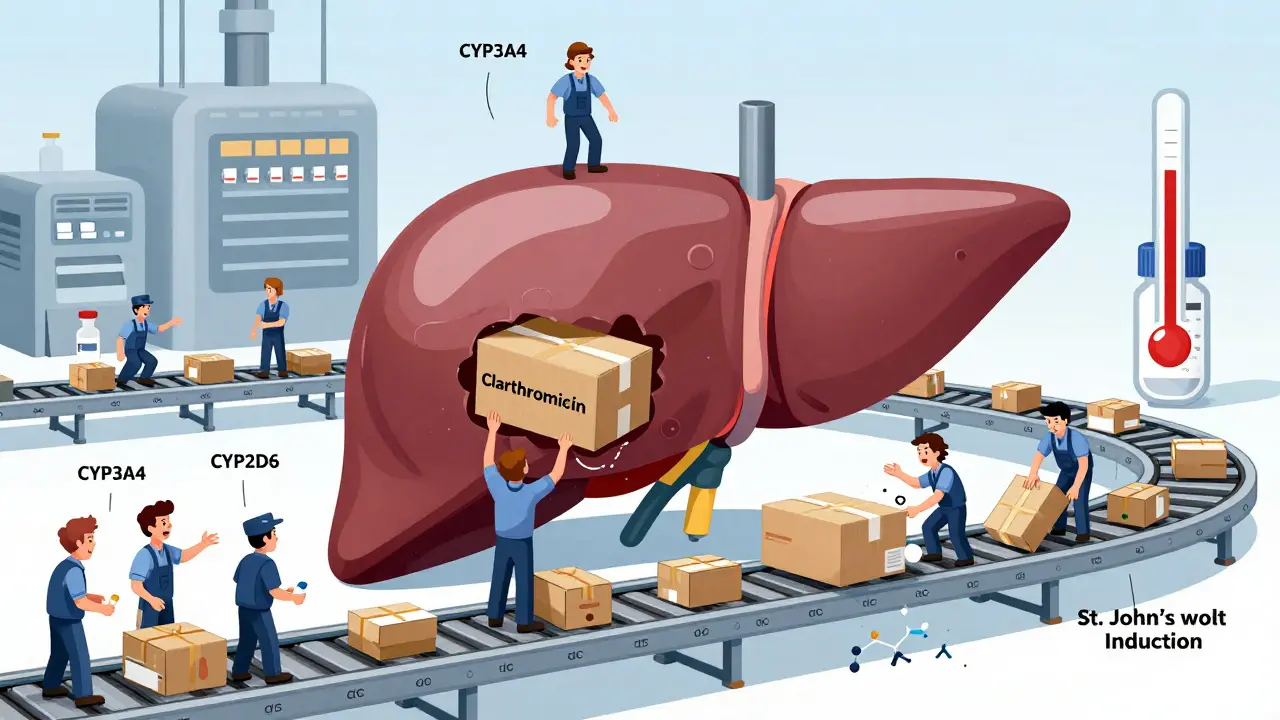
How Drugs Compete: Inhibition vs. Induction
There are two main ways drugs mess with CYP450 enzymes: inhibition and induction.
Inhibition is like jamming the turnstile. One drug sticks to the enzyme and blocks others from getting through. This can happen fast-sometimes within hours. For example, clarithromycin (an antibiotic) is a strong CYP3A4 inhibitor. When someone takes it with simvastatin (a cholesterol drug), the simvastatin can’t be broken down. Levels spike 10-fold. Result? Muscle breakdown, kidney failure, even death. A 2022 case study in the Journal of Clinical Pharmacy and Therapeutics showed exactly this: a 72-year-old woman developed rhabdomyolysis after adding clarithromycin to her simvastatin routine.
Some inhibitors are reversible-meaning they just hang out on the enzyme temporarily. Others are irreversible. These bind permanently, like glue. The enzyme has to be replaced entirely, which takes 3-7 days. That’s why you can’t just stop the inhibitor and expect immediate safety.
Induction is the opposite. It’s like hiring more workers. Certain drugs, like rifampin (an antibiotic used for tuberculosis) or St. John’s wort (a herbal supplement), tell your liver to make more CYP450 enzymes. This doesn’t happen overnight. It takes days to weeks. But once it does, drugs get cleared too fast. For example, if you’re on birth control and start taking St. John’s wort, your body may clear the hormones so quickly that you get pregnant. Or if you’re on an immunosuppressant after a transplant, induction can cause rejection.
Genetics Play a Bigger Role Than You Think
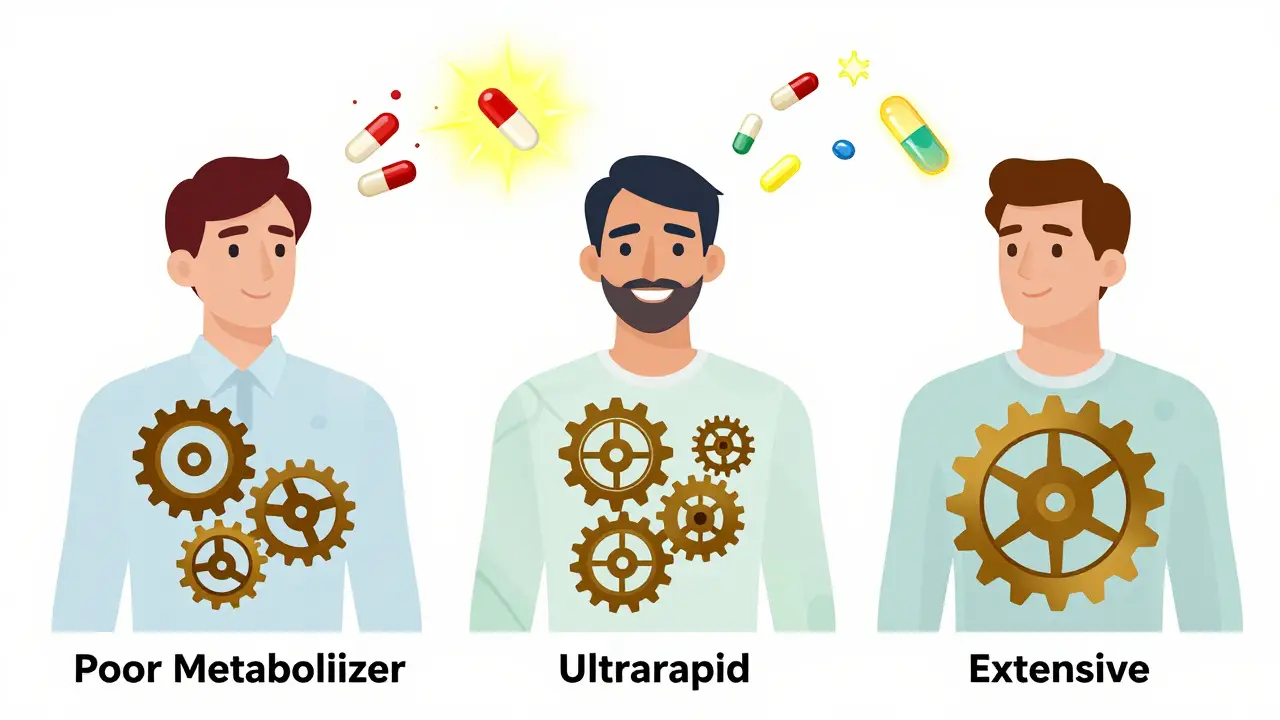
Not everyone processes drugs the same way. Your genes decide whether you’re a slow, normal, or super-fast metabolizer. This is especially true for CYP2D6.
Here’s how it breaks down:
- Poor metabolizers (5-10% of Caucasians): Their CYP2D6 barely works. If they take codeine, it won’t turn into morphine. Pain relief? None. If they take a beta-blocker like metoprolol, it builds up. Heart rate drops dangerously low.
- Ultrarapid metabolizers (1-10%, higher in some populations): They break down drugs too fast. A person on codeine might convert it to morphine so quickly that levels spike, then crash. They get no pain relief and risk overdose.
- Extensive metabolizers (45-50%): The “normal” group. Their enzymes work as expected.
One study found that CYP2D6 genetics explain 40% of why people respond so differently to tricyclic antidepressants. One person needs 25 mg. Another needs 100 mg. Same drug. Same diagnosis. Different genes.
And it’s not just CYP2D6. CYP2C19 affects clopidogrel (Plavix). About 30% of Caucasians and 60% of Asians are poor metabolizers. That means their blood doesn’t thin properly after a heart attack. The FDA now recommends genetic testing before prescribing clopidogrel.
Real-World Cases: What Happens When Things Go Wrong
These aren’t rare exceptions-they’re common clinical disasters.
Case 1: The Theophylline Seizure
A Reddit user named ClinicalPharm87 shared a case where a patient on theophylline (for asthma) started taking fluvoxamine (an antidepressant). Fluvoxamine is a strong CYP1A2 inhibitor. Within 48 hours, theophylline levels jumped from 10 mcg/mL to 25 mcg/mL. Normal range is 10-20. Above 20, seizures can occur. The patient had a seizure. They needed ICU care.
Case 2: The Silent Bradycardia
Nurses on AllNurses.com report that 15-20% of patients on both SSRIs (like paroxetine) and metoprolol (a beta-blocker) develop abnormally slow heart rates. Why? SSRIs inhibit CYP2D6. Metoprolol relies on CYP2D6 to be cleared. When it’s blocked, metoprolol piles up. Heart rate drops. Dizziness. Fainting. Sometimes cardiac arrest.
Case 3: The Invisible Overdose
A 60-year-old man on warfarin (CYP2C9 substrate) started taking fluconazole (an antifungal, a strong CYP2C9 inhibitor). His INR (a measure of blood thinning) shot from 2.5 to 8.0 in three days. He didn’t feel sick. But he bled internally. He needed emergency transfusions. No one knew the interaction was possible-until it was too late.
What You Can Do: Avoiding Dangerous Interactions
There’s no magic bullet-but there are smart steps.
- Know your top 5 drugs. List every pill, patch, and supplement you take. Include herbal stuff like St. John’s wort, garlic, and ginkgo. These all interact.
- Ask about CYP450. When a new drug is prescribed, ask: “Is this processed by CYP3A4 or CYP2D6? Could it interfere with what I’m already taking?”
- Use interaction checkers. Tools like Lexicomp or Micromedex catch 95% of major interactions. Pharmacists use them. You should too.
- Watch for red flags. If you start a new drug and suddenly feel dizzy, nauseous, weak, or have irregular heartbeats, get checked. It might be an interaction.
- Consider genetic testing. If you’re on 5+ meds, especially for heart, mental health, or pain, a CYP450 panel (cost: $250-$500) can save your life. Hospitals like Mayo Clinic and Kaiser now offer this routinely.
Some drugs are especially risky because they have a narrow therapeutic index. That means the difference between a helpful dose and a toxic one is tiny. Warfarin, digoxin, phenytoin, and lithium fall into this group. Even a small change in metabolism can kill.
The Future: AI, EHRs, and Personalized Medicine
The good news? We’re getting better at preventing these interactions.
By 2024, 75% of major electronic health record systems (like Epic and Cerner) now flash warnings when a new drug clashes with a patient’s CYP450 profile. IBM Watson’s AI system, tested in 2023, predicted CYP interactions with 89% accuracy. The NIH is standardizing gene names so labs worldwide can talk the same language.
And it’s not just about drugs. The FDA now requires all new medications to be tested for CYP450 interactions before approval. Labels must clearly state which enzymes are affected.
Still, challenges remain. The average Medicare patient takes 5.4 medications. That’s over 10 potential CYP450 conflicts per person. And we still don’t fully understand 30% of genetic variants.
One thing’s clear: CYP450 interactions aren’t a niche concern. They’re the #1 modifiable cause of preventable drug-related hospitalizations. If you’re on more than three medications, this isn’t theoretical. It’s personal.
Can I still take grapefruit juice if I’m on medication?
It depends on your medication. Grapefruit juice strongly inhibits CYP3A4 in the gut. If you’re taking simvastatin, atorvastatin, felodipine, cyclosporine, or some anti-anxiety drugs, even one glass can raise drug levels by 30-80%. For others, like lisinopril or metformin, it’s fine. Always check with your pharmacist or use an interaction checker.
Are herbal supplements safe with prescription drugs?
No, not necessarily. St. John’s wort induces CYP3A4 and CYP2C9, making birth control, antidepressants, and blood thinners less effective. Garlic and ginkgo can thin your blood and interact with warfarin. Green tea may inhibit CYP3A4. Supplements aren’t regulated like drugs-and many have hidden interactions.
Why do some people need higher doses of the same drug?
It’s often genetics. People who are ultrarapid metabolizers break down drugs too fast and need higher doses. Poor metabolizers clear drugs slowly and can overdose on standard doses. CYP2D6 alone can cause 100-fold differences in drug response between people. That’s why one person needs 5 mg of a beta-blocker, and another needs 50 mg.
How long does it take for a CYP450 interaction to show up?
It varies. Inhibition can happen in hours-like when you take clarithromycin with simvastatin. Induction takes days to weeks. For example, St. John’s wort needs 1-2 weeks to fully induce CYP3A4. And after stopping an inducer, it can take 1-3 weeks for enzyme levels to return to normal.
Is CYP450 testing covered by insurance?
Sometimes. Medicare and many private insurers cover CYP450 testing if you’re on high-risk drugs like clopidogrel, warfarin, or certain antidepressants. Out-of-pocket costs range from $250-$500. If you’re on 5+ medications, the test can prevent costly hospitalizations-making it worth the investment.

Sarah Barrett
February 14, 2026 AT 17:22The way CYP450 enzymes jostle for space like commuters during rush hour is both fascinating and terrifying. I never realized grapefruit juice could turn a routine statin into a ticking time bomb. It’s not just about pills-it’s about the quiet, invisible ballet happening inside our livers every single day. One wrong move, and the whole system stutters. The case studies? Chilling. A 72-year-old woman rhabdomyolyzing because of a simple antibiotic combo? That’s not a rare glitch-it’s a systemic blind spot. We treat drugs like Lego blocks, snapping them together without checking if they’re made of the same plastic.
And yet, we don’t test. We don’t screen. We just prescribe. It’s like driving a car with a blindfold because ‘everyone else does it.’
Josiah Demara
February 14, 2026 AT 19:32Stop romanticizing this as some mysterious biological dance. It’s not poetry-it’s negligence. Pharmacists have had interaction databases for decades. Doctors still prescribe simvastatin with clarithromycin like it’s a lunch special. The fact that this is still happening in 2024 proves the medical system is either incompetent or willfully blind. And don’t get me started on herbal ‘supplements.’ St. John’s wort isn’t ‘natural medicine’-it’s a biochemical grenade with a pull tab labeled ‘unregulated.’
Genetic testing? Only for the wealthy? That’s not healthcare. That’s class-based triage. If your genes make you a poor metabolizer, you’re either lucky enough to afford testing or you’re a statistic. This isn’t science. It’s capitalism with a stethoscope.
Kaye Alcaraz
February 16, 2026 AT 08:42This is one of the most vital explanations of drug metabolism I’ve ever read. Thank you for breaking it down with such clarity. The subway turnstile analogy? Brilliant. It makes the abstract terrifyingly tangible.
For anyone reading this: if you take more than three medications, please sit down with your pharmacist. Not your doctor. Your pharmacist. They are trained specifically for this. They have tools, they have time, and they are not paid to rush. Ask for a med review. Ask about CYP450. Ask if your supplements are safe. It’s not paranoia-it’s empowerment.
And yes, genetic testing is worth it. One test can prevent years of hospital visits, misdiagnoses, and near-fatal events. Your future self will thank you.
Charlotte Dacre
February 17, 2026 AT 10:15So let me get this straight. We’ve known about this since the 80s, but we still let people take St. John’s wort with birth control? And we call this a ‘healthcare system’? I’m not shocked. I’m just disappointed in how creatively we’ve managed to turn science into a game of Russian roulette with side effects.
Next up: ‘Why you shouldn’t drink coffee while on antidepressants.’ Spoiler: it’s not because caffeine’s bad. It’s because your liver is now a hostage situation.
Chiruvella Pardha Krishna
February 18, 2026 AT 05:02Human biology is a labyrinth of hidden rules. We are not machines. We are not equations. We are living, breathing paradoxes shaped by millennia of evolution-and yet, we treat our bodies like software that can be patched with a new app.
The CYP450 system is not merely a metabolic pathway. It is a mirror of our hubris. We believe we can control life with pills, yet we refuse to see that life has its own language, its own rhythm, its own silent laws. To ignore genetics is to deny the soul of medicine. To ignore interactions is to dance on the edge of a cliff and call it progress.
Virginia Kimball
February 18, 2026 AT 23:11I just started a new beta-blocker and was about to pick up St. John’s wort for ‘anxiety relief.’ Then I read this. Holy cow. I almost killed myself without even trying. Thank you for the wake-up call. I’m dumping the herbs, scheduling a med review, and telling my whole family to do the same. This isn’t just info-it’s a lifesaver. Seriously. If you’re on meds, read this twice. Then show it to your mom.
Kapil Verma
February 20, 2026 AT 23:03Western medicine is a joke. We spend billions on pills but refuse to test genes? In India, we’ve known for generations that people react differently to medicine. Our Ayurvedic practitioners never gave the same dose to two patients. Why? Because they knew biology isn’t one-size-fits-all. Now we have science that proves it-and still, the West clings to its outdated protocols like a religious doctrine.
This isn’t about drugs. It’s about arrogance. We think we know better than nature. We don’t.
Michael Page
February 22, 2026 AT 09:13The most disturbing part isn’t the interactions. It’s that we don’t track them systematically. No national database. No mandatory reporting. Just patchwork warnings and hope. If a car part failed this often, the whole industry would be shut down. But people dying from drug interactions? That’s just ‘an unfortunate side effect.’
I wonder how many deaths are buried in ‘cause unknown’ reports. Probably thousands.
Betty Kirby
February 23, 2026 AT 16:01