Compare Furosemide with Alternative Diuretics: What Works Best?
 Nov, 6 2025
Nov, 6 2025
When your body holds onto too much fluid, it can cause swelling, shortness of breath, or high blood pressure. Furosemide is one of the most common pills doctors prescribe to flush out that extra water. But it’s not the only option. Many people end up switching from furosemide - either because it stops working well, causes side effects, or their condition changes. So what are the real alternatives, and how do they actually compare?
What furosemide does and who takes it
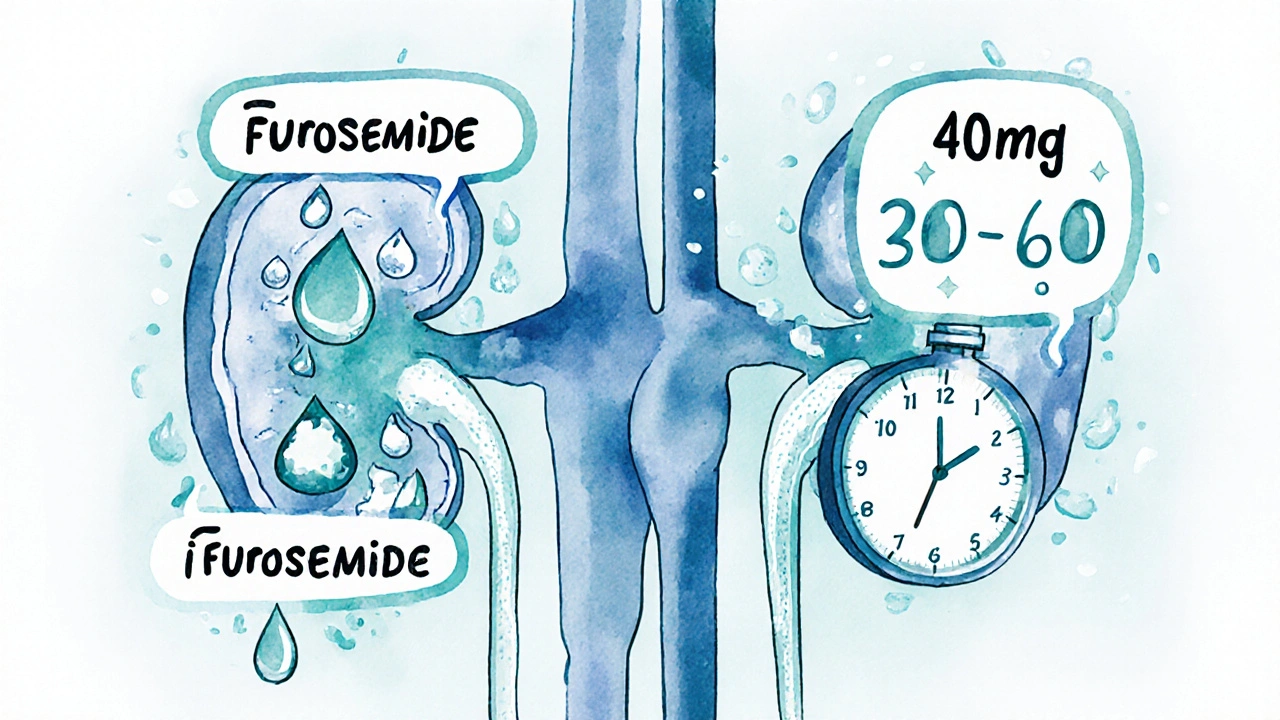
Furosemide is a loop diuretic, which means it works in the loop of Henle in your kidneys. It tells your body to dump sodium and water out through urine. This reduces fluid buildup in conditions like heart failure, liver cirrhosis, kidney disease, and severe high blood pressure. Most people start with 20 to 40 mg once a day, though doses can go higher depending on how much fluid they need to lose.
It works fast - usually within 30 to 60 minutes after taking it orally. The effect lasts about 2 hours, but the diuretic action can keep going for 4 to 6 hours. That’s why many people take it in the morning, to avoid waking up at night to use the bathroom.
Why people switch from furosemide
Not everyone tolerates furosemide well. Some report muscle cramps, dizziness, or low potassium levels. Others find that after months of use, the pill doesn’t move as much fluid as it used to - a sign of diuretic resistance. In these cases, doctors consider switching to another diuretic. Sometimes, they add a second type instead of replacing it entirely.
Here are the three most common alternatives: bumetanide, torsemide, and hydrochlorothiazide. Each has different strengths, timing, and side effect profiles.
Bumetanide: Stronger, shorter, and more predictable
Bumetanide is also a loop diuretic, just like furosemide. But it’s about 40 times more potent. That means a 0.5 mg dose of bumetanide is roughly equal to 20 mg of furosemide. Because it’s so strong, you need smaller doses, which can reduce the risk of electrolyte imbalances.
One big advantage? Bumetanide is absorbed more reliably from the gut. Furosemide’s absorption can drop by up to 50% in people with heart failure or kidney problems. Bumetanide doesn’t have that issue. That makes it a go-to choice when furosemide stops working as expected.
On the downside, bumetanide’s effect doesn’t last as long - about 2 hours. So you might need to take it twice a day. It’s also more expensive and not always covered by insurance without prior authorization.
Torsemide: Longer-lasting and gentler on the kidneys
Torsemide is another loop diuretic, but it’s built to last. Its effects can stretch out for 6 to 8 hours - sometimes even up to 12. That means once-daily dosing is often enough, even at higher strengths. Many patients prefer this because it’s easier to stick with.
Studies show torsemide may be better at reducing hospital readmissions in heart failure patients compared to furosemide. One 2023 analysis of over 12,000 patients found those on torsemide had 22% fewer hospital stays for worsening heart failure over 12 months.
Torsemide also has a lower risk of causing low magnesium and low potassium than furosemide. It’s metabolized by the liver, not the kidneys, so it’s often chosen for people with reduced kidney function. The downside? It’s pricier than furosemide and may require a specialty pharmacy.
Hydrochlorothiazide: A different kind of diuretic
Hydrochlorothiazide (HCTZ) isn’t a loop diuretic - it’s a thiazide. It works lower down in the kidney, in the distal convoluted tubule. That means it’s weaker than furosemide. You’d need 50 mg of HCTZ to match the fluid removal of 40 mg of furosemide.
But here’s the twist: HCTZ is often used alongside furosemide, not instead of it. In heart failure patients, combining a thiazide with a loop diuretic can break through diuretic resistance. It’s called sequential nephron blockade. One study showed that adding 50 mg of HCTZ to furosemide increased urine output by 30% in patients who weren’t responding to furosemide alone.
HCTZ is cheap, widely available, and often used for high blood pressure. But it’s not strong enough on its own for severe fluid overload. It can also raise blood sugar and uric acid levels, so it’s avoided in people with gout or uncontrolled diabetes.
Comparison table: Furosemide vs. alternatives
| Feature | Furosemide | Bumetanide | Torsemide | Hydrochlorothiazide |
|---|---|---|---|---|
| Class | Loop diuretic | Loop diuretic | Loop diuretic | Thiazide diuretic |
| Typical starting dose | 20-40 mg | 0.5-1 mg | 10-20 mg | 12.5-25 mg |
| Onset of action | 30-60 min | 30-60 min | 60-120 min | 2 hours |
| Duration of effect | 4-6 hours | 2-4 hours | 6-12 hours | 6-12 hours |
| Peak effect time | 1-2 hours | 1-2 hours | 2-4 hours | 4-6 hours |
| Half-life | 1-2 hours | 1 hour | 3-4 hours | 6-15 hours |
| Dosing frequency | 1-2 times daily | 1-2 times daily | Once daily | Once daily |
| Best for | General fluid overload | Diuretic resistance, poor absorption | Heart failure, once-daily need | Mild hypertension, combo therapy |
| Cost (30-day supply) | $5-$15 | $25-$50 | $30-$70 | $4-$10 |
When to choose which alternative
Choosing between these options isn’t about which one is “better.” It’s about matching the drug to your body and your condition.
- If furosemide isn’t working anymore and you have heart failure or kidney problems, try bumetanide. It’s more reliable when your body isn’t absorbing meds well.
- If you want to take just one pill a day and avoid frequent bathroom trips, torsemide is often the best pick. It’s also preferred if your kidneys are already struggling.
- If you’re on furosemide but still retaining fluid, your doctor might add hydrochlorothiazide instead of increasing your furosemide dose. This combo is proven to work better than higher doses of either alone.
- If cost is a big issue and you have mild swelling, furosemide or HCTZ are still first-line choices.
What not to do
Don’t switch diuretics on your own. Changing from furosemide to torsemide or bumetanide isn’t as simple as swapping pills. Doses don’t match up one-to-one. Taking too much bumetanide can cause dangerous drops in blood pressure or potassium. Too much torsemide can lead to dehydration or kidney stress.
Also, don’t assume a “stronger” diuretic is always better. Torsemide and bumetanide aren’t more effective at saving lives - they’re just better suited for certain situations. Furosemide still works great for millions of people.
Side effects to watch for
All diuretics can cause:
- Low potassium (can lead to muscle weakness or irregular heartbeat)
- Low sodium (can cause confusion or falls)
- Dehydration (dizziness, dry mouth, dark urine)
- Increased uric acid (may trigger gout)
Torsemide and bumetanide may cause slightly less potassium loss than furosemide. HCTZ is more likely to raise blood sugar and cholesterol. If you’re on any of these, your doctor should check your blood levels every few months.
What’s next if none of these work?
If you’re still retaining fluid despite trying multiple diuretics, your doctor may consider:
- Adding a potassium-sparing diuretic like spironolactone - often used with furosemide in heart failure
- Using ultrafiltration - a machine that removes fluid directly from your blood
- Adjusting your salt intake, fluid limits, or other heart/kidney medications
Can I switch from furosemide to torsemide on my own?
No. Torsemide is not a direct substitute for furosemide. A 40 mg dose of furosemide is roughly equal to 10-20 mg of torsemide, but the conversion isn’t exact. Switching without medical supervision can lead to under- or over-diuresis, which can be dangerous. Always consult your doctor before changing diuretics.
Is bumetanide stronger than furosemide?
Yes, bumetanide is about 40 times more potent than furosemide. A 1 mg dose of bumetanide equals roughly 40 mg of furosemide. This makes it useful when you need strong diuresis with smaller doses, especially if furosemide isn’t being absorbed well due to heart or kidney disease.
Why does furosemide stop working over time?
This is called diuretic resistance. It happens when your kidneys adapt to the drug by reabsorbing more sodium. It’s common in people with advanced heart failure or kidney disease. Adding a second diuretic like hydrochlorothiazide or switching to torsemide can help overcome this.
Can I take hydrochlorothiazide instead of furosemide for swelling?
Only if the swelling is mild. Hydrochlorothiazide is much weaker than furosemide. For severe fluid buildup from heart failure or liver disease, it’s not strong enough on its own. But it’s often added to furosemide to boost results.
Which diuretic is safest for long-term use?
Torsemide is often considered the safest for long-term use in heart failure because it has a longer duration, requires once-daily dosing, and causes fewer electrolyte disturbances than furosemide. But safety depends on your kidney function, diet, and other medications. Regular blood tests are essential no matter which one you take.
Final thoughts
Furosemide has been the go-to diuretic for decades - and for good reason. But medicine doesn’t stand still. Torsemide offers longer, steadier relief. Bumetanide gives you more control when absorption is a problem. Hydrochlorothiazide helps when you need a gentle nudge, not a flood.
The best choice isn’t the one you’ve always taken. It’s the one that matches your body’s needs right now. Talk to your doctor about your symptoms, side effects, and goals. There’s no one-size-fits-all diuretic. Your treatment should evolve as your health does.

Beth Banham
November 8, 2025 AT 01:22Been on furosemide for 3 years and honestly? Torsemide was a game changer. One pill a day, no midnight bathroom runs, and my swelling finally stopped creeping back. My doc switched me after I hit diuretic resistance - no drama, just better results.
Also, side effects? Way less crampy. I used to wake up with leg cramps like a horror movie. Now? Just a quiet morning and coffee.
Don’t let cost scare you - my insurance covered it after one appeal. Worth it.
Brierly Davis
November 9, 2025 AT 05:02Yessss!! Torsemide saved my life 😊 I was on 80mg furosemide twice a day and still puffy as a balloon. Switched to 20mg torsemide - one pill, same results, no more midnight marathons to the bathroom. My wife says I sleep like a baby now 🛌
Also, my potassium levels actually stayed normal? Wild. Doc said it’s because torsemide doesn’t hammer your kidneys as hard. Big win.
Amber O'Sullivan
November 9, 2025 AT 15:41Furosemide is outdated and overused like a 2005 iPhone. Bumetanide is the real upgrade and anyone still prescribing furosemide as first line is just lazy. My cardiologist switched me after 6 months of no progress and now I’m stable. Stop being cheap and start being smart. Also HCTZ as a solo move for edema? That’s not treatment that’s a joke.
Jim Oliver
November 11, 2025 AT 05:02Wow. Someone actually wrote a coherent article without saying 'consult your doctor' 47 times. Shocking. But let’s be real - if you’re still using furosemide after 2024, you’re either on Medicare or your doctor still uses fax machines. Torsemide isn’t 'better' - it’s just not broken. Bumetanide? Yes. HCTZ combo? Smart. Everything else? Band-aids on a hernia.
William Priest
November 11, 2025 AT 15:58so like... furosemide is so last decade? like why even bother? torsemide is the real MVP, its like the tesla of diuretics. bumetanide? yeah its strong but its expensive like a starbucks latte every day. and hctz? nope. not for real swelling. its for people who think their ankles are 'a little puffy' after eating tacos. i mean... come on.
Ryan Masuga
November 11, 2025 AT 21:33Just wanted to say - if you’re reading this and you’re struggling with diuretics, you’re not alone. I was on furosemide for years, felt like a ghost, and thought I’d never feel normal again. Then my doc added HCTZ and everything changed. It’s not magic, but it’s real. Your body adapts, but so can your treatment. Don’t give up. Talk to your team. There’s a combo out there for you. You got this 💪
Jennifer Bedrosian
November 13, 2025 AT 05:01OMG I switched to torsemide last month and I CRIED I WAS SO HAPPY like I actually slept through the night for the first time in 5 years and my shoes dont feel like concrete blocks and my husband said I stopped sighing every time I stood up and I just want to hug everyone who wrote this post because I thought I was the only one suffering like this
Lashonda Rene
November 14, 2025 AT 02:43i just want to say that i think everyone is right in their own way because i was on furosemide for a long time and it stopped working and then my doctor tried bumetanide and it made me feel dizzy so then we tried torsemide and it was better but then my potassium got low so now we are doing torsemide with a potassium pill and sometimes we add hctz if i get really swollen and its not perfect but its better than before and i think the point is that its different for everyone and you have to try stuff and listen to your body and dont get mad at your doctor if they dont have all the answers right away because medicine is complicated and your body changes and thats okay
Andy Slack
November 14, 2025 AT 15:36One sentence: Torsemide > Furosemide for long-term use. Period.