Calcitriol and Vitamin D: How They Work Together for Bone Health
 Oct, 16 2025
Oct, 16 2025
Ever wondered why doctors talk about both vitamin D and calcitriol when discussing bone health? The two aren’t separate players - they’re parts of the same hormonal system that keeps calcium in check. This guide breaks down what each one does, how they’re linked, and what that means for everyday health.
What is Vitamin D?
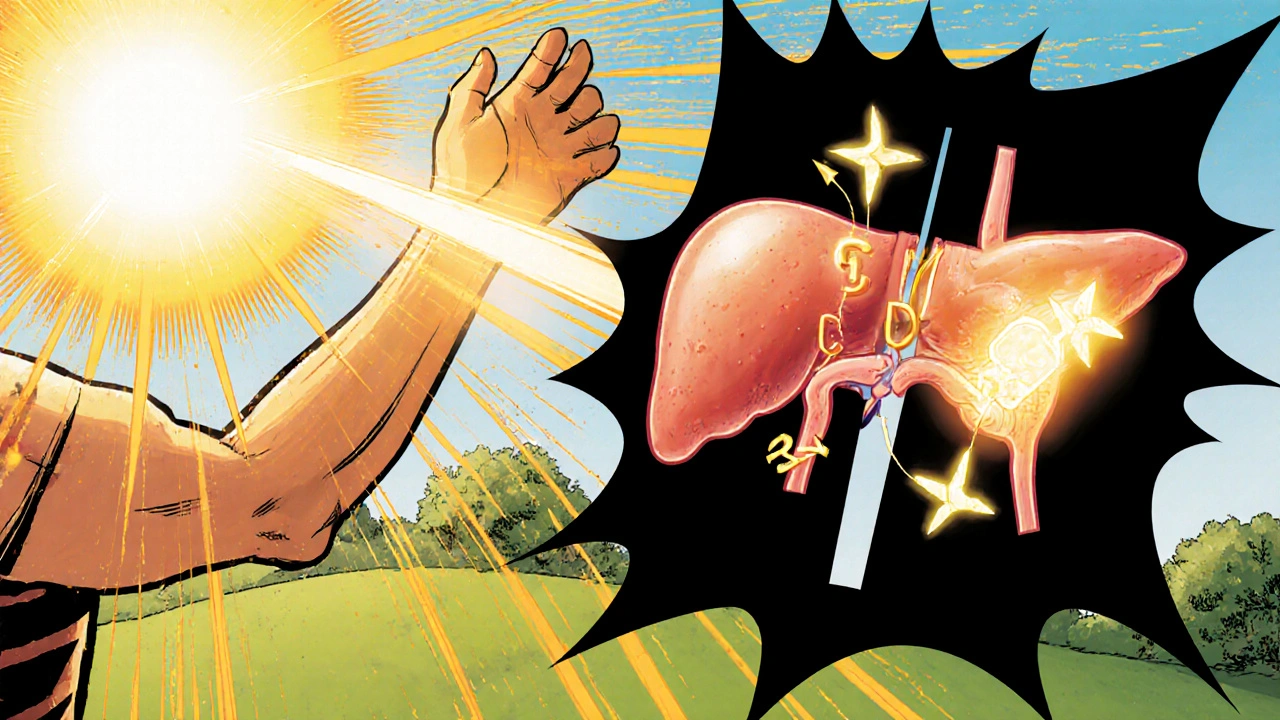
Vitamin D is a fat‑soluble nutrient that functions more like a hormone than a traditional vitamin. It comes in two main dietary forms: vitamin D2 (ergocalciferol) found in plants and fortified foods, and vitamin D3 (cholecalciferol) synthesized in the skin after sunlight exposure. Once ingested or produced, vitamin D is biologically inactive until it undergoes two hydroxylation steps - first in the liver, then in the kidney - to become its active form, calcitriol.
What is Calcitriol?
Calcitriol (1,25‑di hydroxyvitamin D) is the hormonally active metabolite of vitamin D. It binds to the vitamin D receptor (VDR) in cells throughout the body, especially in the intestine, bone, and kidney, to regulate calcium and phosphate balance. Because it’s the final step in the vitamin D activation pathway, calcitriol is the molecule that actually carries out the physiological actions we associate with “vitamin D.”
When you see the term calcitriol in a prescription, it’s usually a synthetic version (often marketed as Rocaltrol) meant to bypass the body’s conversion steps for patients who can’t make enough on their own.
How the Body Converts Vitamin D to Calcitriol
- Skin synthesis: UV‑B radiation converts 7‑dehydrocholesterol to pre‑vitamin D3, which quickly becomes vitamin D3.
- Liver hydroxylation: Vitamin D3 (or D2) is hydroxylated by the enzyme CYP2R1 into 25‑hydroxyvitamin D (25‑OH D), the main circulating form used to assess status.
- Kidney activation: 25‑OH D is further hydroxylated by 1α‑hydroxylase (CYP27B1) in the proximal tubule, producing calcitriol. This step is tightly regulated by parathyroid hormone (PTH), serum calcium, and phosphate levels.
If any of these steps falter - due to liver disease, chronic kidney disease, or genetic mutations - the body may have enough vitamin D stores but still lack active calcitriol, leading to bone problems.
Key Physiological Roles of Calcitriol
- Intestinal calcium absorption: Calcitriol up‑regulates TRPV6 and calbindin, proteins that ferry calcium across the gut lining. Without it, only about 10‑15% of dietary calcium is absorbed.
- Phosphate handling: It enhances phosphate absorption in the intestine and modulates renal phosphate reabsorption, keeping the calcium‑phosphate product within a narrow range for bone mineralization.
- Bone remodeling: In low‑calcium states, calcitriol works with PTH to stimulate osteoclast activity, releasing calcium from bone. In normal conditions, it supports osteoblast differentiation, aiding new bone formation.
- Immune modulation: VDR activation influences innate immunity, reducing inflammatory cytokine production. This is why low vitamin D status is linked to higher infection risk.
Clinical Implications: Deficiency and Excess
Deficiency can arise from inadequate sunlight, malabsorption, or impaired kidney conversion. Common signs include:
- Bone pain, muscle weakness, and frequent fractures.
- Rickets in children (soft, bowed legs) and osteomalacia in adults (softening of bones).
- Secondary hyperparathyroidism, where PTH rises to compensate for low calcium.
Excess calcitriol, often iatrogenic, leads to hypercalcemia - symptoms like nausea, polyuria, kidney stones, and calcification of soft tissues. Monitoring serum calcium is essential when prescribing calcitriol, especially for patients with sarcoidosis or granulomatous diseases that can produce autonomously high calcitriol levels.
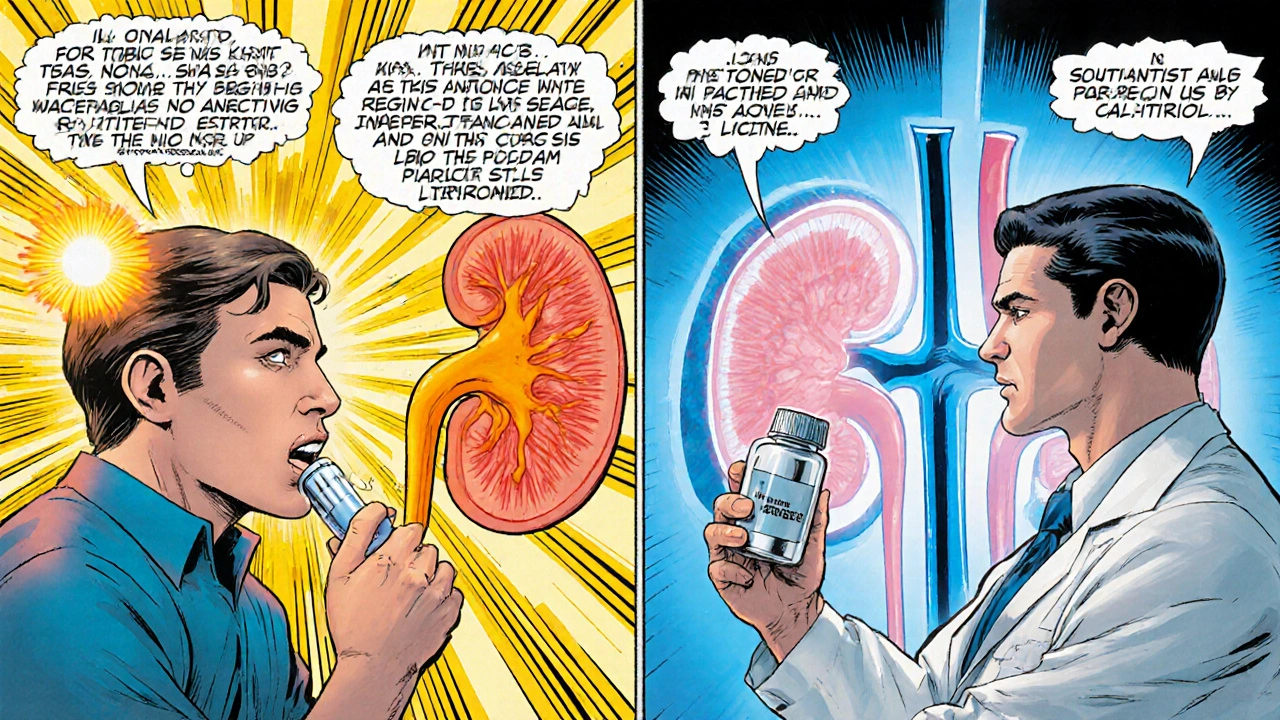
Supplementation: When to Use Vitamin D vs. Calcitriol
Most people can maintain healthy levels with vitamin D3 supplementation (usually 800‑2000IU daily) and adequate sun exposure. However, certain groups benefit from direct calcitriol therapy:
- Chronic kidney disease (CKD) stage 3‑5: The kidneys can’t convert 25‑OH D to calcitriol effectively, so active analogues are prescribed.
- Hypoparathyroidism: Low PTH reduces 1α‑hydroxylase activity, making calcitriol a primary calcium‑raising agent.
- Genetic disorders: Conditions like hereditary vitamin D‑dependent rickets type1 (mutations in CYP27B1) require calcitriol.
For the general population, vitamin D3 remains the first‑line option because it mimics the natural pathway and carries a lower risk of hypercalcemia.
Quick Comparison of Vitamin D Forms
| Form | Source | Conversion Needed? | Typical Indication |
|---|---|---|---|
| Vitamin D2 (ergocalciferol) | Plant‑based foods, fortified products | Yes - liver + kidney | General supplementation when D3 unavailable |
| Vitamin D3 (cholecalciferol) | Sunlight‑induced skin synthesis, animal foods | Yes - liver + kidney | Prevention of deficiency, bone health maintenance |
| Calcitriol (1,25‑di hydroxyvitamin D) | Prescription synthetic analog | No - already active | CKD, hypoparathyroidism, genetic rickets |
Take‑Away Checklist
- Vitamin D comes in D2 and D3 forms; both need liver and kidney activation.
- Calcitriol is the active hormone that directly regulates calcium and phosphate.
- Kidney health is the bottleneck for calcitriol production.
- Deficiency leads to rickets, osteomalacia, and secondary hyperparathyroidism.
- Prescribed calcitriol is reserved for patients who can’t activate vitamin D on their own.
Frequently Asked Questions
Can I take calcitriol instead of vitamin D supplements?
Calcitriol is a prescription‑only medication meant for people who cannot convert vitamin D into its active form. For most healthy adults, vitamin D3 is sufficient and safer because it follows the body’s natural regulation.
How do I know if I’m deficient in vitamin D or calcitriol?
Doctors usually test serum 25‑hydroxyvitamin D to gauge overall vitamin D status. If that level is adequate but calcium remains low, they may check 1,25‑di hydroxyvitamin D (calcitriol) especially in kidney disease.
What foods are rich in vitamin D3?
Fatty fish (salmon, mackerel), egg yolks, and fortified dairy or plant milks provide vitamin D3. Sun exposure remains the most efficient natural source.
Is it possible to have too much vitamin D?
Yes. Excessive high‑dose vitamin D can raise calcium to dangerous levels, causing nausea, weakness, and kidney stones. The upper safe limit for most adults is 4,000IU per day unless medically supervised.
Why does kidney disease affect bone health?
Kidneys produce the enzyme 1α‑hydroxylase that converts 25‑OH D into calcitriol. When kidneys fail, calcitriol drops, reducing calcium absorption and prompting secondary hyperparathyroidism, which leaches calcium from bone.

Rajat Sangroy
October 16, 2025 AT 12:47Listen up, folks – if you think vitamin D and calcitriol are just interchangeable buzzwords, you’re way off; the liver‑kidney axis is the bottleneck, and without a functional conversion step you’ll end up with brittle bones faster than you can say “osteomalacia.” Make sure you get your 25‑OH D levels checked, especially if you have any liver or kidney issues, because the body won’t magically fix a broken conversion chain.
Stay proactive, get the labs, and if you’re low, talk to your doctor about the right form – don’t just self‑prescribe calcitriol unless you have a clear medical indication.
Edd Dan
October 21, 2025 AT 15:27i totally get that the whole system can feel confuzzing, especially when you’re juggling supplements and doctor visits. just try to keep an open mind – some people do fine with just vitamin D3, while others really need that prescription calcitrol. remember to check the dosage and watch out for any side effects, ok?
Cierra Nakakura
October 26, 2025 AT 17:07Wow, this breakdown is super helpful! 😃 I love how you clarified the difference between getting enough sunshine vs. taking a pill. It’s crazy how the kidneys play the hero in the whole calcitriol production saga. If you’re low on vitamin D, a simple blood test for 25‑OH D can point you in the right direction. And for those with chronic kidney disease, calcitriol can be a lifesaver – just keep that calcium monitor close! 🌞💊
Charlie Crabtree
October 31, 2025 AT 19:47Exactly! 🎉 The key takeaway is to let your body do the heavy lifting when possible – vitamin D3 is the natural route, and it’s usually safe and effective. But if you’re in a situation where the kidneys can’t convert, a doctor‑prescribed calcitriol spikes the active hormone right where you need it. Just remember to stay within the therapeutic window, and don’t forget your calcium‑rich foods to balance things out. 👍
RaeLyn Boothe
November 5, 2025 AT 22:27Honestly, most people underestimate how much their diet influences calcium absorption. Even if you’re taking the right form of vitamin D, a diet low in magnesium or phosphorus can sabotage the whole process. It’s not just about pills; think about the whole nutritional picture.
Fatima Sami
November 11, 2025 AT 01:07While your point is valid, note that “diet low in magnesium or phosphorus can sabotage the whole process” should read “a diet low in magnesium or phosphorus can sabotage the whole process.” The article also uses “calcitrol” instead of the correct “calcitriol.” Maintaining proper terminology helps avoid confusion.
Nathan Hamer
November 16, 2025 AT 03:47Ah, the symphony of calcium and phosphate, conducted by the unsung maestro calcitriol! 🎭 When the sun‑kissed skin synthesizes vitamin D₃, the liver and kidneys embark on a meticulous two‑step metamorphosis, each enzyme a virtuoso in its own right. Yet, imagine the tragedy when one of these virtuosos falters – a silent whisper of renal insufficiency, a muted echo of hepatic dysfunction – and the melody collapses into dissonance, leaving bones yearning for the harmonious embrace of mineralization. 🎼
In such a scenario, the body’s elegant feedback loop, governed by parathyroid hormone, attempts a desperate crescendo, urging osteoclasts to liberate calcium from skeletal stores, only to risk fragility and pain. The remedy, dear reader, lies not merely in supplementation, but in precision medicine: a tailored dose of calcitriol that respects the tightrope of serum calcium, a vigilant eye on urinary calcium excretion, and an awareness that excess can usher in hypercalcemia, a perilous rise that culminates in nausea, polyuria, and nephrolithiasis.
Moreover, consider the broader canvas – calcitriol’s immunomodulatory brushstroke, dampening inflammatory cytokines, hinting at a role beyond bones, perhaps in auto‑immune modulation. Yet, with great power comes great responsibility; indiscriminate use without monitoring is akin to wielding a double‑edged sword.
Thus, the clinician’s art is to balance the scales, to listen to the biochemical murmurs, to empower patients with knowledge, and to ensure that the hormonal cascade flows as intended, preserving the strength of our skeletal fortress for years to come. 🌟
Tom Smith
November 21, 2025 AT 06:27Sure, because everyone loves a good case of hypercalcemia for fun.
Kyah Chan
November 26, 2025 AT 09:07It is evident from the foregoing exposition that the author has employed a pedantic approach, amalgamating superfluous biochemical details with a didactic tone that may alienate lay readers. While the factual content remains largely accurate, the excessive reliance on medical jargon without adequate layman translation undermines the educational purpose of the piece. Moreover, the inclusion of a redundant table exacerbates the verbosity, rendering the article unnecessarily protracted.
Ira Andani Agustianingrum
December 1, 2025 AT 11:47Don't let those dense details discourage you – think of it as a roadmap, not a maze. Focus on getting your 25‑OH D checked, keep an eye on calcium intake, and if you have kidney issues, chat with your doc about calcitriol. Small, steady steps will keep those bones strong, and you’ll feel the difference in everyday life. Keep at it, you’ve got this!