Bisacodyl vs. Other Laxatives: How to Choose the Right One
 Oct, 19 2025
Oct, 19 2025
Laxative Selector Tool
Find the Right Laxative for You
Answer a few questions about your situation to get personalized recommendations based on medical guidelines.
When constipation strikes, the sheer number of over‑the‑counter options can feel overwhelming. You might wonder whether to reach for a tablet, a powder, or a gentle oil‑based option. This guide breaks down bisacodyl and compares it with the most common laxatives so you can pick the one that matches your body and lifestyle.
What Is Bisacodyl?
Bisacodyl is a synthetic stimulant laxative that works by irritating the lining of the colon, prompting a wave of muscle contractions (peristalsis) that push stool out. It’s been on the market since the 1950s and is sold under brand names like Dulcolax and Correctol. Typical adult doses range from 5 mg to 10 mg taken orally, with effects appearing in 6‑12 hours. For rapid relief, a suppository form can work within 15‑60 minutes.
How Do Other Laxatives Work?
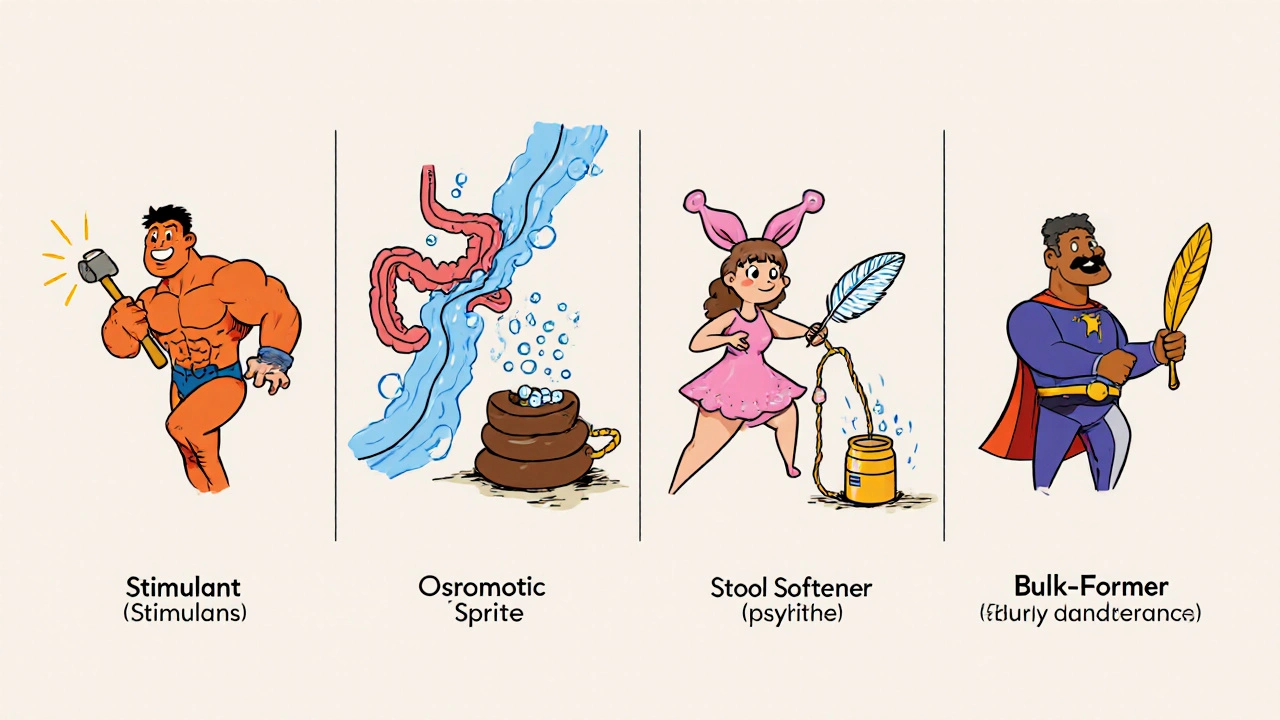
Not all laxatives push stool out the same way. Broadly, they fall into four categories:
- Stimulant laxatives - trigger intestinal muscles (e.g., bisacodyl, senna).
- Osmotic laxatives - draw water into the colon (e.g., polyethylene glycol, lactulose, magnesium hydroxide).
- Stool softeners - lower surface tension so water can coat stool (e.g., docusate sodium).
- Bulk‑forming agents - add fiber to increase stool volume (e.g., psyllium husk).
Each class has a different onset time, side‑effect profile, and ideal use case.
Key Players in the Laxative Landscape
Below are the most widely used alternatives to bisacodyl, each introduced with a microdata definition.
Docusate sodium is a stool softener that moistens the stool by increasing its water content. It’s popular for people who need gentle relief, especially after surgery.
Polyethylene glycol (often sold as PEG 3350) is an osmotic laxative that retains water in the bowel, softening stool and increasing volume. It’s the active ingredient in products like Miralax.
Senna is a plant‑derived stimulant laxative that works similarly to bisacodyl by stimulating colonic nerves. It’s available as tablets, teas, and liquid extracts.
Lactulose is an osmotic laxative made from synthetic sugars that draws water into the colon and also reduces ammonia levels in the blood. It’s often prescribed for chronic constipation and hepatic encephalopathy.
Magnesium hydroxide (commonly called milk of magnesia) is an osmotic laxative that works by increasing the osmotic pressure inside the intestine. It can be taken as a liquid or chewable tablet.
Psyllium husk is a bulk‑forming fiber supplement that absorbs water, expands, and adds bulk to stool, encouraging natural peristalsis. It’s the main ingredient in Metamucil.
Side‑Effect Snapshot
Every laxative carries potential downsides. Here’s a quick look:
- Bisacodyl - abdominal cramps, urgency, electrolyte loss if overused.
- Docusate sodium - generally mild; occasional oily stools or nausea.
- Polyethylene glycol - bloating, gas, rare allergic reactions.
- Senna - cramping, possible melanosis coli with long‑term use.
- Lactulose - extensive gas, sweet taste, may cause diarrhea.
- Magnesium hydroxide - cramping, risk of hypermagnesemia in renal failure.
- Psyllium husk - bloating, must be taken with enough fluid to avoid blockage.
Comparison Table
| Product | Class | Typical Onset | Common Dose | Pros | Cons |
|---|---|---|---|---|---|
| Bisacodyl | Stimulant | 6‑12 h (oral), 15‑60 min (suppository) | 5‑10 mg oral, 10 mg suppository | Reliable, works for occasional severe constipation | Cramping, possible electrolyte loss |
| Docusate sodium | Stool softener | 12‑72 h | 100 mg 1‑2×/day | Gentle, safe for long‑term use | May be ineffective for hard stools |
| Polyethylene glycol (PEG 3350) | Osmotic | 1‑3 days | 17 g powder dissolved in 8 oz water | Predictable, can be used for chronic constipation | Gas, bloating |
| Senna | Stimulant | 6‑12 h | 17‑34 mg (1‑2 tablets) daily | Fast acting, plant‑based | Cramping, risk of pigment changes with long use |
| Lactulose | Osmotic | 24‑48 h | 15‑30 mL (sweet syrup) once daily | Also reduces ammonia for liver patients | Extensive gas, sweet taste |
| Magnesium hydroxide | Osmotic | 30‑60 min | 5‑15 mL liquid or 2‑4 tablets | Quick relief, inexpensive | Risk of hypermagnesemia in kidney disease |
| Psyllium husk | Bulk‑forming | 12‑24 h | 1‑2 Tbsp mixed in water | Supports regular bowel health, natural | Must drink plenty of fluid; can cause bloating |
Choosing the Right Laxative: Decision Guide
Use the flow below to match your situation with the best option.
- Need fast relief (under a few hours)? Go for bisacodyl suppositories, magnesium hydroxide, or a stimulant tablet (senna).
- Prefer a gentle, daily maintenance solution? Choose docusate sodium, psyllium husk, or low‑dose PEG.
- Have kidney disease or are on diuretics? Avoid magnesium‑based products and high‑dose stimulant laxatives; stick with stool softeners or fiber.
- Pregnant or breastfeeding? Docusate sodium and psyllium are generally considered safe; consult a clinician before using stimulant laxatives.
- History of electrolyte imbalance? Limit bisacodyl and other stimulants; opt for osmotic agents that are less likely to cause shifts.
Remember, the goal isn’t just to push anything out; it’s to restore a regular, comfortable rhythm.

Practical Tips to Maximize Effectiveness
- Take laxatives with a full glass of water unless the label says otherwise.
- Never combine two stimulant laxatives at the same time.
- For fiber supplements, start with a small dose and gradually increase to avoid gas.
- Store tablets in a cool, dry place to maintain potency.
- If you need relief for more than three consecutive days, seek medical advice to rule out underlying conditions.
When to See a Doctor
Constipation that lasts longer than two weeks, is accompanied by severe abdominal pain, vomiting, or blood in the stool warrants professional evaluation. Chronic constipation may signal IBS, thyroid disorders, or neurological issues that need targeted treatment.
Frequently Asked Questions
Can I use bisacodyl every day?
Bisacodyl is intended for short‑term use. Daily use for more than a week can lead to dependence and electrolyte imbalance. If you need regular relief, discuss a maintenance plan with a healthcare provider.
Is it safe to take bisacodyl with other medications?
Bisacodyl can speed up drug absorption, so it may affect how quickly other oral meds work. Separate the timing by at least 2 hours, especially for heart or anti‑seizure drugs.
How does a stool softener differ from a stimulant?
A stool softener like docusate adds moisture to the stool, making it easier to pass without triggering strong contractions. A stimulant such as bisacodyl actively prompts the colon muscles to contract, producing a quicker, more forceful evacuation.
Can I use PEG while on a low‑sodium diet?
PEG does not contain sodium, so it’s generally safe for low‑sodium diets. However, always verify the label for any added electrolytes and discuss with a dietitian if you have strict restrictions.
What’s the best way to prevent constipation long term?
Aim for 25‑30 grams of fiber daily (fruits, vegetables, whole grains), stay hydrated (about 2 liters of water), and incorporate regular movement. Use laxatives only when lifestyle tweaks aren’t enough.
Whether you choose bisacodyl, a gentle stool softener, or an osmotic powder, the key is matching the product to your body’s needs and using it responsibly. With the right information, you can keep constipation under control without unnecessary side effects.

Christian Georg
November 1, 2025 AT 13:26Just a heads‑up, take bisacodyl with a full glass of water 👍.
Leo Chan
November 13, 2025 AT 03:13Great rundown! I’ve tried the bisacodyl suppository when I was stuck on a road trip and it really saved the day. For everyday maintenance, I stick to docusate and a bit of psyllium – they’re gentle and keep things moving without the panic attacks. If you have any kidney issues, definitely steer clear of magnesium‑based stuff; the article nailed that point. Remember to stay hydrated, especially if you’re loading up on fiber. Keep sharing these practical guides, they’re super helpful!
jagdish soni
November 24, 2025 AT 17:00One must appreciate the subtle hierarchy that governs the pharmacodynamics of laxatives, bisacodyl sitting atop a throne of synthetic ingenuity. Its mechanism, a gentle irritant to the colonic mucosa, provokes peristalsis with a finesse that few natural agents can mimic. Compare this to senna, a plant‑derived cousin that sacrifices elegance for raw vigor, often leaving the user with a souvenir of cramping. The osmotic class, exemplified by polyethylene glycol, operates on the principle of water influx, a principle so elementary yet profoundly effective. Yet, the elegance of osmotic pull pales when faced with the urgency of a suppository that bypasses the gastric gauntlet entirely. Magnesium hydroxide, the humble milk of magnesia, provides swift relief but at the cost of a possible electrolyte dance in the renally impaired. Docusate, the oft‑overlooked emollient, whispers rather than shouts, moistening the stool without inciting muscular contraction. Psyllium, the bulk‑forming sage, invites the colon to work its natural rhythm, demanding respect for adequate hydration. The side‑effect tableau reads like a cautionary tale, each class bearing its own scarlet flag. Bisacodyl’s cramps are a reminder that stimulation is not without price; electrolyte loss can be a silent thief in prolonged use. Senna’s potential for melanosis coli is a botanical caution, a pigmentary reminder of chronic overuse. PEG’s bloating may be dismissed as trivial but can compromise comfort in the delicate balance of gut flora. Lactulose, with its saccharine overture, delivers gas in generous portions, a comedic side‑effect that masks its therapeutic value. The author’s decision matrix correctly aligns urgency with stimulant choices, yet neglects a nuanced view of patient compliance. In practice, the choice must be tailored, respecting comorbidities, lifestyle, and the ever‑present specter of dependence. Ultimately, knowledge of these mechanisms empowers the consumer to wield the appropriate agent with confidence, avoiding the pitfalls of blanket self‑medication.
Latasha Becker
December 6, 2025 AT 06:46While the guide is thorough, it glosses over the fact that many over‑the‑counter laxatives lack rigorous clinical validation for chronic use. The assertion that docusate is “generally safe” ignores multiple studies showing limited efficacy beyond placebo. Moreover, the recommendation to “never combine two stimulant laxatives” could be nuanced-certain short‑term regimens actually benefit from synergistic action under medical supervision. The table also omits dosage adjustments for pediatric patients, a glaring oversight given the prevalence of constipation in children. Finally, the statement that PEG does not contain sodium is technically correct but neglects formulations that embed electrolytes for enhanced rehydration. A more critical appraisal would serve readers better than the current optimistic tone.
parth gajjar
December 17, 2025 AT 20:33Honestly this article reads like a pharmacy catalog not a real-life guide the tone is too sterile you need more of the lived experience of battling that stubborn blockage. Bisacodyl may work but the cramping can feel like a punch in the gut making the whole process miserable. I’ve tried magnesium hydroxide after a night out and woke up with a rush you wouldn’t believe. The fiber tip is solid however if you don’t drink enough water the psyllium will just sit there ready to clog you further. Spice it up with personal anecdotes next time.
Madhav Dasari
December 29, 2025 AT 10:20Nicely put Leo! I totally agree that staying hydrated is the cornerstone, especially when you bulk up with psyllium. Adding a quick walk after a dose can also boost motility without any extra meds. Keep the encouragement coming, it really helps newcomers navigate the options.
DHARMENDER BHATHAVAR
January 10, 2026 AT 00:06Your points are well taken; the efficacy of docusate indeed remains contentious, and pediatric dosing warrants explicit mention. Adjusting the guide to reflect these nuances would enhance its clinical reliability.
Kevin Sheehan
January 21, 2026 AT 13:53In the grand theater of gastrointestinal stewardship, such pedantic nitpicking borders on intellectual hubris; the article’s purpose is to empower, not to drown readers in academic minutiae. While precision matters, an overly critical lens can obscure the practical wisdom that ultimately liberates the constipated individual.