Benzodiazepines and Opioids: The Deadly Risk of Combined Respiratory Depression
 Dec, 4 2025
Dec, 4 2025
When you take an opioid for pain and a benzodiazepine for anxiety, you might think you’re just managing two separate problems. But what you’re really doing is stacking two drugs that can shut down your breathing-slowly, silently, and sometimes fatally. This isn’t a rare accident. It’s a predictable, well-documented, and deadly pattern that’s killed thousands in the last decade.
Why This Combination Is So Dangerous
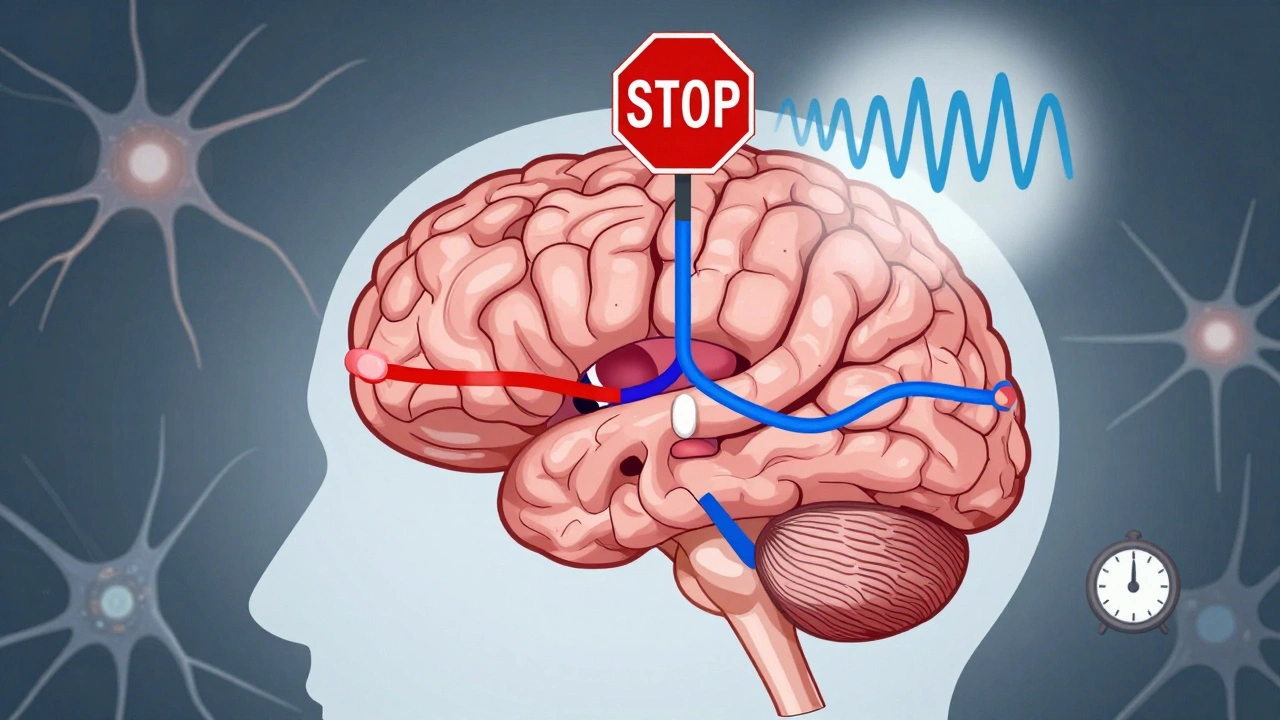
Opioids like oxycodone, hydrocodone, or fentanyl work by binding to mu-opioid receptors in your brainstem. These receptors control the automatic rhythm of your breathing. When activated, they slow down the signal that tells your lungs to inhale. The result? Shallow breaths, longer pauses between breaths, and eventually, complete respiratory arrest. Benzodiazepines-like alprazolam, lorazepam, or diazepam-work differently, but with the same deadly outcome. They boost GABA, the brain’s main calming chemical. This doesn’t just make you relaxed; it suppresses the entire central nervous system, including the parts of your brain that keep you breathing. Alone, a therapeutic dose of a benzo might cause drowsiness. But when paired with an opioid, the effect isn’t just added-it’s multiplied. A 2018 study in the Journal of Pharmacology and Experimental Therapeutics found that when fentanyl and midazolam were given together, minute ventilation dropped by 78%. Alone, fentanyl cut it by 45%. Midazolam alone? Just 28%. That’s not a 73% increase-it’s a near-total collapse of breathing capacity. The brainstem doesn’t just get quieter; it goes silent.The Science Behind the Silence
Research from 2021, published in PMC8424565, shows opioids don’t just slow breathing-they distort it. They lengthen the exhale phase, making each breath feel like a struggle to start again. This happens because opioids act on the Kölliker-Fuse/Parabrachial complex, a region that controls expiration. At the same time, they silence key neurons in the preBötzinger Complex, the brain’s breathing rhythm generator. Benzodiazepines amplify this by flooding the same areas with extra GABA inhibition. They hit the preBötzinger Complex and the Kölliker-Fuse region too, making it even harder for your brain to restart breathing after an exhale. The result? You stop breathing. And because both drugs act on overlapping brain circuits, the suppression isn’t linear-it’s exponential. This isn’t theory. It’s autopsy data. The CDC reports that in 2019, benzodiazepines were found in 17% of opioid overdose deaths involving prescription opioids, and in 22.5% of those involving illicit opioids like heroin or fentanyl. In 2020, that number stayed stubbornly high-16% of all opioid-related deaths still involved benzos.Who’s at Risk-and Why It’s Not Just Drug Users
You might assume this only happens with recreational use. But most deaths occur in people prescribed both drugs by doctors. A landmark 2016 study in JAMA Internal Medicine found that patients taking both opioids and benzodiazepines had a 10 times higher risk of dying from an overdose than those taking opioids alone. These weren’t people buying drugs off the street. These were patients with chronic pain and anxiety-people following their prescriptions, trusting their doctors. The highest risk group? People aged 45 to 64. Often, they’re on long-term opioids for back pain or arthritis, and prescribed benzos for insomnia or panic attacks. Their bodies are slower to metabolize drugs. Their lungs are less resilient. And their brains are more vulnerable to the combined suppression. Even one pill can be enough. A 65-year-old woman taking oxycodone for osteoarthritis and lorazepam for sleep might not feel “high.” She might just feel tired. But her breathing is already dangerously suppressed. One missed dose of either drug, a cold that makes her cough, or even lying flat on her back at night can be the trigger that stops her breathing for good.
What Doctors Are Supposed to Do-And What They Often Don’t
The FDA issued a black box warning in 2016-the strongest possible alert-saying that combining these drugs can cause coma and death. The CDC’s 2016 prescribing guidelines say: Avoid concurrent use whenever possible. The American Society of Anesthesiologists says the same: Avoid it. But prescribing patterns don’t change overnight. In 2022, a study in the American Journal of Public Health found that even after the FDA warning, 8.7% of patients on long-term opioids were still being prescribed benzodiazepines. That’s nearly one in ten. Some doctors still believe benzos help with opioid withdrawal or improve sleep. Others don’t know the full risk. Many patients don’t know either. Prescription drug monitoring programs (PDMPs) now flag risky combinations in 16 states. Medicare Part D has rules to catch high-risk prescriptions. But these systems are reactive, not preventive. By the time the system flags you, you may already be in danger.What to Do Instead
If you’re on an opioid and struggling with anxiety or insomnia, you don’t have to risk your life. For anxiety: Buspirone is a non-addictive alternative that doesn’t suppress breathing. SSRIs like sertraline or escitalopram are effective for chronic anxiety and don’t interact dangerously with opioids. For insomnia: Cognitive behavioral therapy for insomnia (CBT-I) is the gold standard-and it works better than sleeping pills long-term. Melatonin, sleep hygiene, and light therapy are safer, non-drug options. For pain: Non-opioid options like physical therapy, acupuncture, NSAIDs (if safe for you), or nerve blocks can reduce or eliminate the need for opioids altogether. If you absolutely must take both drugs-say, for severe, treatment-resistant conditions-your doctor should use the lowest possible doses for the shortest time. They should monitor you closely. You should have naloxone on hand. And you should never take these drugs with alcohol or sleep aids.
Naloxone Doesn’t Fix Everything
Naloxone saves lives when opioids cause overdose. But it does nothing for benzodiazepine-induced respiratory depression. If you’re overdosing on both, naloxone might bring back your breathing for a few minutes-but then it shuts down again because the benzo is still in your system. That’s why emergency responders now carry higher doses of naloxone and are trained to watch for signs of benzo involvement. But even that’s not enough. A 2022 study in the Journal of Neurophysiology showed that an experimental drug called CX1739 could reverse combined respiratory depression in animals. It’s not available to the public yet. Until better treatments arrive, the only reliable protection is prevention.The Bigger Picture
Between 1999 and 2019, deaths from combined opioid and benzodiazepine overdoses rose by 1,800%. In 2023, the CDC estimated 12,000 to 15,000 people in the U.S. alone will die this way. These aren’t just numbers. They’re parents, siblings, coworkers. People who trusted the system. We’ve made progress. Prescribing rates have dropped 14.5% since the FDA warning. But we’re still losing people because the message hasn’t reached everyone. Patients still take both drugs because they’re told it’s “normal.” Doctors still prescribe them because they’re unaware of the full danger. This isn’t about fear. It’s about facts. And the facts are clear: combining benzodiazepines and opioids is one of the most predictable and preventable causes of death in modern medicine. If you’re on either drug-or both-talk to your doctor. Ask: Is this combination really necessary? Ask: What are the safer alternatives? And if you’re unsure, get naloxone. Keep it in your home. Teach your family how to use it. Because sometimes, the only thing standing between you and a fatal overdose is knowing the risk-and acting before it’s too late.Can you overdose on opioids and benzodiazepines even if you take them as prescribed?
Yes. Many overdose deaths occur in people who take both drugs exactly as directed by their doctors. The danger comes from the way these drugs interact in the brainstem, not from taking too much. Even therapeutic doses can combine to dangerously suppress breathing, especially in older adults or people with lung conditions.
Does naloxone work if someone overdoses on both opioids and benzodiazepines?
Naloxone can reverse the opioid part of the overdose, but it does nothing for the benzodiazepine. This means breathing may improve briefly after naloxone is given, but it can shut down again as the benzo continues to suppress the brain. Emergency medical care is always needed-even after naloxone is administered.
Are there safe alternatives to benzodiazepines for anxiety if I’m on opioids?
Yes. Buspirone is a non-addictive anti-anxiety medication that doesn’t affect breathing. SSRIs like sertraline or escitalopram are also effective for chronic anxiety and have no dangerous interaction with opioids. Non-drug treatments like cognitive behavioral therapy (CBT) are often more effective long-term and carry no physical risk.
Why do doctors still prescribe both drugs together?
Some doctors aren’t fully aware of the risk, especially if they’re treating long-term pain and anxiety. Others believe benzos help with opioid withdrawal or improve sleep. But guidelines from the CDC, FDA, and American Society of Anesthesiologists all warn against it. If your doctor prescribes both, ask why and what safer options exist.
Can I stop one of these drugs on my own?
No. Stopping opioids or benzodiazepines suddenly can cause dangerous withdrawal symptoms, including seizures or rebound anxiety. Always work with your doctor to taper safely. If you’re concerned about the combination, talk to them about switching to safer alternatives before making any changes.

Katie Allan
December 5, 2025 AT 03:30This post is one of those rare pieces that doesn’t just inform-it changes how you see medicine. I’ve seen too many older patients on oxycodone and lorazepam because ‘it’s what the doctor said.’ No one ever told them the breathing risk wasn’t just theoretical. It’s not about fearmongering. It’s about giving people the facts so they can ask the right questions. If your doctor prescribes both, ask for alternatives. Buspirone. CBT-I. SSRIs. There are options. Your life isn’t worth the convenience of two pills.
And if you’re reading this and you’re on both-don’t panic. But do talk to someone. Today.
Someone’s parent, sibling, or friend could be reading this right now. And maybe this is the moment they realize they’re not alone in being scared.
Kylee Gregory
December 5, 2025 AT 16:44I’ve worked in palliative care for 18 years. I’ve watched people die from this exact combination-quietly, in their sleep, with their family beside them, and no one realizing it was the meds, not the illness. The tragedy isn’t that people took them. It’s that no one ever told them this was a death sentence waiting to happen. The system failed them. Not because anyone was malicious, but because the warnings never made it past the prescription pad.
Doctors are overworked. Patients are told ‘this is normal.’ We need better education, not just warnings on a label. This isn’t just a drug interaction-it’s a cultural blind spot.
Lucy Kavanagh
December 6, 2025 AT 09:47Let me guess-this is all part of the pharmaceutical industry’s plan to keep people dependent. They don’t want you cured, they want you on pills forever. Why else would they push this combo? Look at the numbers-they’ve been dropping since 2016, but only because the government started pushing ‘safer alternatives.’ But guess what? Those alternatives are just more drugs. Buspirone? Still made by Big Pharma. CBT? Too expensive for the working class. This whole thing is a distraction. The real issue? The FDA and CDC are controlled by lobbyists. You think they care about your breathing? They care about profits.
And don’t get me started on naloxone. That’s just a Band-Aid. They don’t want to fix the system. They want you to think you’re safe while they keep selling the poison.
Stephanie Fiero
December 7, 2025 AT 06:46As a nurse who’s seen this firsthand-this is the most important thing I’ve read all year. I had a patient, 62, on oxycodone for back pain and Xanax for panic attacks. She didn’t even know they could kill her. She thought the ‘sleepiness’ was just aging. We found out when she stopped breathing during a nap. Naloxone brought her back-but she was in the ICU for a week. She cried when she realized she almost died because her doctor never told her.
So I started handing out pamphlets. I tell every patient on opioids: ‘If you’re on a benzo, ask your doctor if you really need it.’ No one ever says no. But they start asking questions. That’s the win.
Also-CBT-I works. I did it myself after my divorce. Better sleep than pills. And no risk of dying in your sleep.
PLEASE-share this. Someone you love might be reading this and not know.
Philip Kristy Wijaya
December 7, 2025 AT 23:36Also why is everyone so obsessed with prescribing alternatives when the real issue is that people keep asking for the same drugs over and over again?
Jennifer Patrician
December 8, 2025 AT 07:23Okay so let me get this straight-Big Pharma and the FDA are letting people die so they can sell more SSRIs and CBT programs? That’s the real agenda here. CBT? That’s a cult. They don’t want you healed-they want you dependent on therapists who charge $200/hour. And buspirone? It’s a placebo with a fancy name. The real reason they’re pushing this is because they’re trying to get rid of benzodiazepines so they can sell you antidepressants instead. And guess what? Antidepressants have their own deadly side effects. This whole thing is a scam. They’re not trying to save lives-they’re trying to control your mind.
And don’t even get me started on naloxone. That’s just a way to keep addicts alive so they keep buying drugs. Why not just let nature take its course? If you can’t handle your anxiety and pain without pills, maybe you shouldn’t be alive. This isn’t compassion. It’s enabling.
Mellissa Landrum
December 9, 2025 AT 02:06My cousin died from this. He was on oxycodone for his back and Xanax for his anxiety. He took them exactly like the doctor said. No alcohol. No street drugs. Just two pills a day. He went to bed one night and never woke up. The coroner said it was respiratory depression from the combo. The doctor never warned him. The pharmacy never flagged it. The system failed him. And now his kids are growing up without a dad because no one cared enough to say ‘this could kill you.’
So yeah-this isn’t theory. This is my family. And I’m tired of people acting like this is just a statistic. It’s not. It’s someone’s son. Someone’s brother. Someone’s best friend. If you’re on both drugs-ask your doctor. Now. Don’t wait until it’s too late.
And if you’re a doctor reading this-stop being lazy. You have a duty. This isn’t hard. Look at the guidelines. They’ve been there for years.
luke newton
December 10, 2025 AT 20:39