Antiemetics and Parkinson’s Medications: Avoiding Dangerous Dopamine Interactions
 Jan, 29 2026
Jan, 29 2026
Why Your Anti-Nausea Medicine Could Make Parkinson’s Worse
If you or someone you care for has Parkinson’s disease and gets nauseous from levodopa, you might be handed a common antiemetic like metoclopramide or prochlorperazine without realizing the risk. These drugs are sold over the counter in some places and given routinely in hospitals for vomiting or stomach upset. But for Parkinson’s patients, they can trigger sudden stiffness, freezing, tremors, or even hospitalization. The problem isn’t the nausea-it’s the cure.
Parkinson’s disease slowly destroys dopamine-producing cells in the brain. That’s why patients take levodopa: to replace what’s lost. But many anti-nausea drugs work by blocking dopamine receptors. When those drugs reach the brain, they fight against levodopa’s effect, making symptoms worse. It’s like turning off the lights while trying to read a book with a dim bulb.
The Drugs That Can Trigger a Parkinson’s Crisis
Not all anti-nausea meds are dangerous. But some are ticking time bombs for Parkinson’s patients. The biggest offenders are dopamine D2 receptor blockers:
- Metoclopramide (Reglan, Maxalon) - Often prescribed for post-op nausea or diabetic gastroparesis. Despite being used for decades, it crosses the blood-brain barrier and can cause sudden worsening of movement symptoms. One patient on a Parkinson’s forum described it as "turning my body to stone" after a dental procedure.
- Prochlorperazine (Stemetil) - Common in emergency rooms. Can cause acute dystonia, rigidity, and prolonged "off" periods. A 2022 survey found 22% of Parkinson’s patients who got this drug needed hospital care.
- Haloperidol (Haldol) - Used for psychosis or severe agitation. Extremely high risk. Even small doses can trigger neuroleptic malignant syndrome, a life-threatening reaction.
- Chlorpromazine and Promethazine - Found in many sleep aids and allergy meds. Both block dopamine and are on the American Parkinson Disease Association’s "Medications to Avoid" list.
These drugs are still widely prescribed because they’re cheap, effective for nausea, and many doctors don’t know the Parkinson’s connection. A 2022 study showed only 37% of ER doctors could identify metoclopramide as risky for Parkinson’s patients.
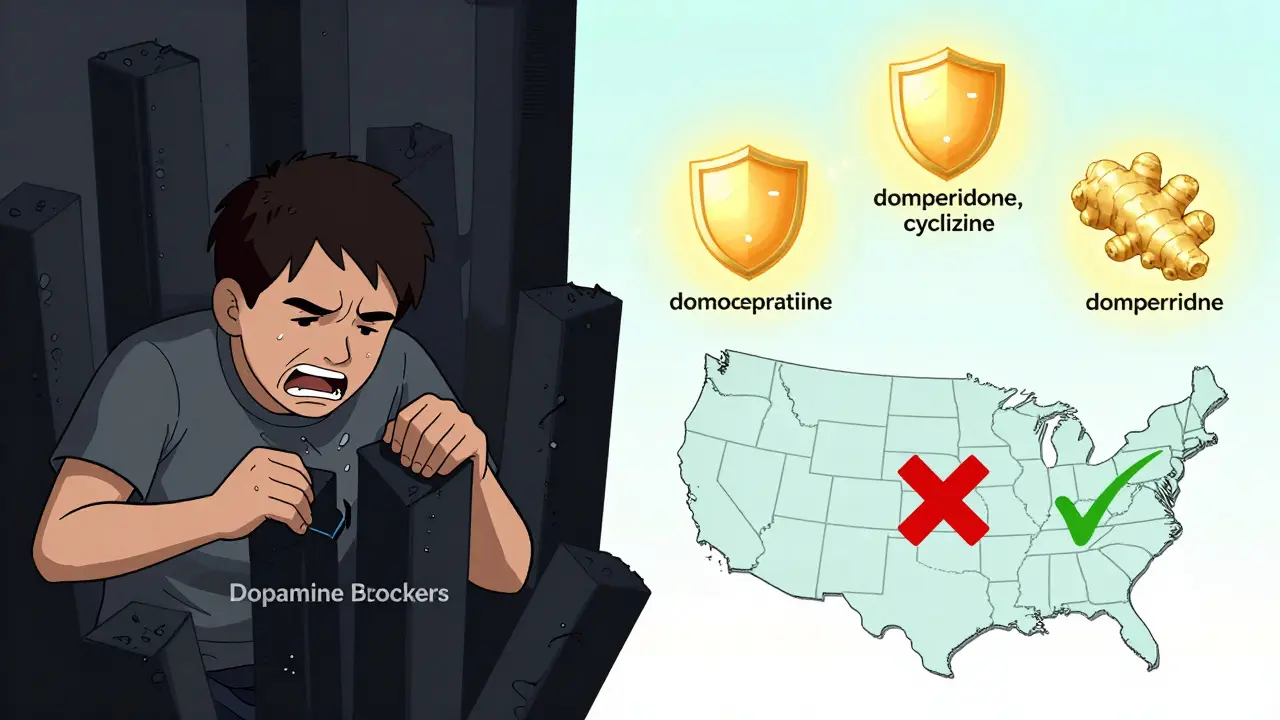
The Safer Alternatives That Actually Work
You don’t have to suffer through nausea. There are safer options that don’t touch dopamine in the brain.
- Domperidone (Motilium) - This is the gold standard for Parkinson’s patients. It blocks dopamine in the gut to stop nausea but can’t cross the blood-brain barrier because of a natural "pump" that pushes it out. Risk of worsening symptoms? Less than 2%. The catch? It’s not available as an injection in the U.S. and requires special approval from the FDA.
- Cyclizine (Vertin) - An antihistamine that works on the inner ear and nausea centers without touching dopamine. Studies show only 5-10% risk of worsening motor symptoms. One Reddit user said switching from metoclopramide to cyclizine ended his weekly freezing episodes.
- Ondansetron (Zofran) - Blocks serotonin, not dopamine. Safe for Parkinson’s, but it doesn’t work as well for all types of nausea, especially those caused by stomach delay.
- Ginger - A natural option backed by research. Taking 1 gram daily in capsule or tea form reduces nausea in 60% of Parkinson’s patients. No drug interactions. No side effects. Worth trying before pills.
Levomepromazine (Nozamine) sits in the middle. It has moderate dopamine-blocking power. Only use it if specialists agree, start low (6.25 mg twice daily), and never exceed 25 mg a day.
What Happens When You Get the Wrong Drug
The consequences aren’t theoretical. They’re lived.
A woman in Auckland had dental surgery and was given metoclopramide for nausea. Within hours, her tremors exploded. Her walking froze. She couldn’t speak clearly. It took three weeks of increasing her levodopa dose and waiting for the drug to clear before she returned to baseline. Her neurologist called it "a textbook case of dopamine blockade."
Another patient in the UK was given prochlorperazine in an emergency room. He had a severe "off" period that lasted 48 hours. His family had to call an ambulance. He spent five days in the hospital. His wife said, "They treated the nausea, but they broke my husband."
Data from the Michael J. Fox Foundation shows 68% of Parkinson’s patients who received dopamine-blocking antiemetics in hospitals had clear worsening of symptoms. Over 20% needed longer stays. That’s not a side effect-it’s a medical error.
How to Protect Yourself
Here’s how to avoid this trap:
- Carry a wallet card. The American Parkinson Disease Association gives out free cards listing dangerous drugs. Keep one in your wallet. Show it to every doctor, nurse, and pharmacist.
- Ask: "Is this a dopamine blocker?" If the answer is yes, say no. Ask for an alternative.
- Never accept metoclopramide, prochlorperazine, or haloperidol unless your neurologist says so. Even then, it should be a last resort.
- Use domperidone if you can. In New Zealand, Australia, and Europe, it’s available by prescription. In the U.S., you may need to apply through the FDA’s expanded access program.
- Track your symptoms. If you start feeling stiffer, slower, or more tremulous after taking a new med, stop it and call your doctor immediately.
Some clinics now add a note to prescriptions: "Parkinson’s disease: verify antiemetic safety." That’s a good sign. Push for it.

What’s Changing for the Better
There’s hope. More doctors are learning. The Parkinson’s Foundation trained over 1,200 providers in 2023 and cut inappropriate prescriptions by 55% in their partner hospitals.
New drugs are coming. Aprepitant (Emend), which blocks a different nausea pathway, showed 92% effectiveness in a 2023 trial with zero motor side effects. The Michael J. Fox Foundation is funding a new drug designed specifically for Parkinson’s nausea-no brain penetration, just gut relief.
The American Geriatrics Society now lists metoclopramide as "potentially inappropriate" for Parkinson’s patients. That’s a big deal. It means hospitals and insurers are starting to treat this as a safety issue, not just a recommendation.
Bottom Line: Don’t Let Nausea Cost You Your Movement
Nausea from levodopa is common. But the solution isn’t to reach for the first antiemetic on the shelf. It’s to choose wisely. The wrong drug can undo weeks of progress. The right one can let you eat, travel, and live without fear.
Domperidone. Cyclizine. Ginger. These aren’t just alternatives-they’re your shield. Metoclopramide. Prochlorperazine. Haloperidol. These aren’t just drugs-they’re risks you don’t need to take.
If your doctor prescribes something for nausea, ask: "Will this make my Parkinson’s worse?" If they hesitate, get a second opinion. Your movement matters more than a quick fix.
Can I take metoclopramide if I have Parkinson’s disease?
No. Metoclopramide crosses the blood-brain barrier and blocks dopamine receptors, which can suddenly worsen tremors, stiffness, and freezing in Parkinson’s patients. Even short-term use can trigger severe symptoms. It’s on the American Parkinson Disease Association’s "Medications to Avoid" list. Safer alternatives like domperidone or cyclizine exist.
Is domperidone safe for Parkinson’s patients?
Yes. Domperidone blocks dopamine only in the gut, not the brain, because it can’t cross the blood-brain barrier. It’s one of the safest antiemetics for Parkinson’s, with less than 2% risk of worsening symptoms. It’s widely used in Europe, Australia, and New Zealand. In the U.S., it’s only available through special FDA access programs due to heart rhythm concerns at high doses, not because of Parkinson’s risks.
Why do doctors still prescribe metoclopramide to Parkinson’s patients?
Many doctors aren’t trained in Parkinson’s care. Metoclopramide is cheap, widely available, and effective for nausea in the general population. Emergency rooms and surgeons often default to it. A 2022 study found 62% of Parkinson’s patients received unsafe antiemetics in hospitals. The gap is in education, not availability of safer options.
What should I do if I’ve already taken metoclopramide?
Stop taking it immediately. Contact your neurologist. Symptoms like increased tremor, rigidity, or freezing usually improve within days as the drug leaves your system. You may need to temporarily increase your levodopa dose under medical supervision. Document what happened and share it with all future providers to prevent recurrence.
Are there any non-drug ways to manage nausea with Parkinson’s?
Yes. Start with ginger-1 gram daily in capsule or tea form. Eat small, frequent meals instead of large ones. Stay hydrated. Avoid greasy or spicy foods. Take levodopa on an empty stomach if possible, but if nausea prevents that, talk to your doctor about adjusting the timing or formulation. Many patients find relief just by changing how and when they eat.
Can I use over-the-counter nausea meds like Pepto-Bismol?
Pepto-Bismol (bismuth subsalicylate) is generally safe for Parkinson’s patients because it doesn’t affect dopamine receptors. It’s not as strong as prescription antiemetics, but it’s fine for mild nausea. Avoid any OTC products containing promethazine, dimenhydrinate, or diphenhydramine-they can block dopamine and worsen symptoms.

Blair Kelly
January 30, 2026 AT 19:20This is the kind of post that should be mandatory reading for every ER doc, dentist, and pharmacist in the country. I had a cousin on levodopa who got metoclopramide after a colonoscopy and spent three days in the ICU because they didn’t know the difference between stomach nausea and dopamine blockade. This isn’t a side effect-it’s negligence dressed up as standard care.
Rohit Kumar
January 31, 2026 AT 11:06In India, we see this every day. Doctors prescribe prochlorperazine without a second thought because it’s cheap and fast. No one asks about Parkinson’s unless the patient says it outright. And even then, many don’t believe it’s a real concern. Education is the real medicine here-not just the drugs.
Lily Steele
February 1, 2026 AT 06:21My dad was given metoclopramide after surgery and he couldn’t walk for a week. I didn’t know why until I found this post. Thank you for listing domperidone. We got it through a special program last month and he’s finally eating again without shaking. Just wanted to say-this info saves lives.
Gaurav Meena
February 1, 2026 AT 13:32When I first read this, I thought it was too good to be true. But after switching my mom from prochlorperazine to cyclizine, her freezing episodes dropped from daily to once a month. Ginger tea helped too. It’s not magic-it’s just science that got buried under convenience. We need more awareness, not more pills.
Jodi Olson
February 3, 2026 AT 08:51Domperidone isn’t approved in the U.S. because of QT prolongation risk at high doses not because it’s unsafe for Parkinson’s patients. The FDA’s stance is a regulatory artifact, not a clinical one. The real failure is the lack of pharmaceutical investment in dopamine-sparing antiemetics designed for neurodegenerative populations.
Carolyn Whitehead
February 5, 2026 AT 04:28My grandma took ginger every morning and it helped so much. She said it tasted like home. No hospital drama. Just quiet relief. Maybe we don’t need all the fancy drugs if we just listen to the simple stuff.
Amy Insalaco
February 6, 2026 AT 21:47It’s fascinating how the pharmacodynamics of dopamine receptor antagonism in the basal ganglia creates a paradoxical exacerbation of motor symptoms despite peripheral efficacy. The blood-brain barrier permeability differential between domperidone and metoclopramide is a textbook example of pharmacokinetic optimization, yet clinicians still default to the cheaper, more accessible-but neurotoxic-option. This isn’t just ignorance; it’s systemic devaluation of neurologic patient autonomy.
Katie and Nathan Milburn
February 6, 2026 AT 23:35Just wanted to add: my wife and I both have Parkinson’s. We carry the APDA wallet card everywhere. Last month, a nurse tried to give my wife promethazine for nausea. I showed her the card. She apologized and called the pharmacy. That’s the kind of small moment that changes everything.
Beth Beltway
February 7, 2026 AT 03:18People who say ginger works are just deluding themselves. This isn’t a wellness blog. This is neuroscience. If you’re not using domperidone or ondansetron under strict supervision, you’re gambling with your motor function. And don’t get me started on ‘natural remedies’-they’re placebo traps for the uninformed.
Marc Bains
February 7, 2026 AT 12:30My brother is a neurologist. He told me 80% of the nurses he trains still don’t know metoclopramide is dangerous for Parkinson’s. So I started handing out printed flyers at local clinics. One nurse cried and said she’d given it to three patients last year. We need to stop waiting for guidelines. We need to start teaching.