Acotiamide and Its Role in Treating Esophageal Motility Disorders
 Oct, 28 2025
Oct, 28 2025
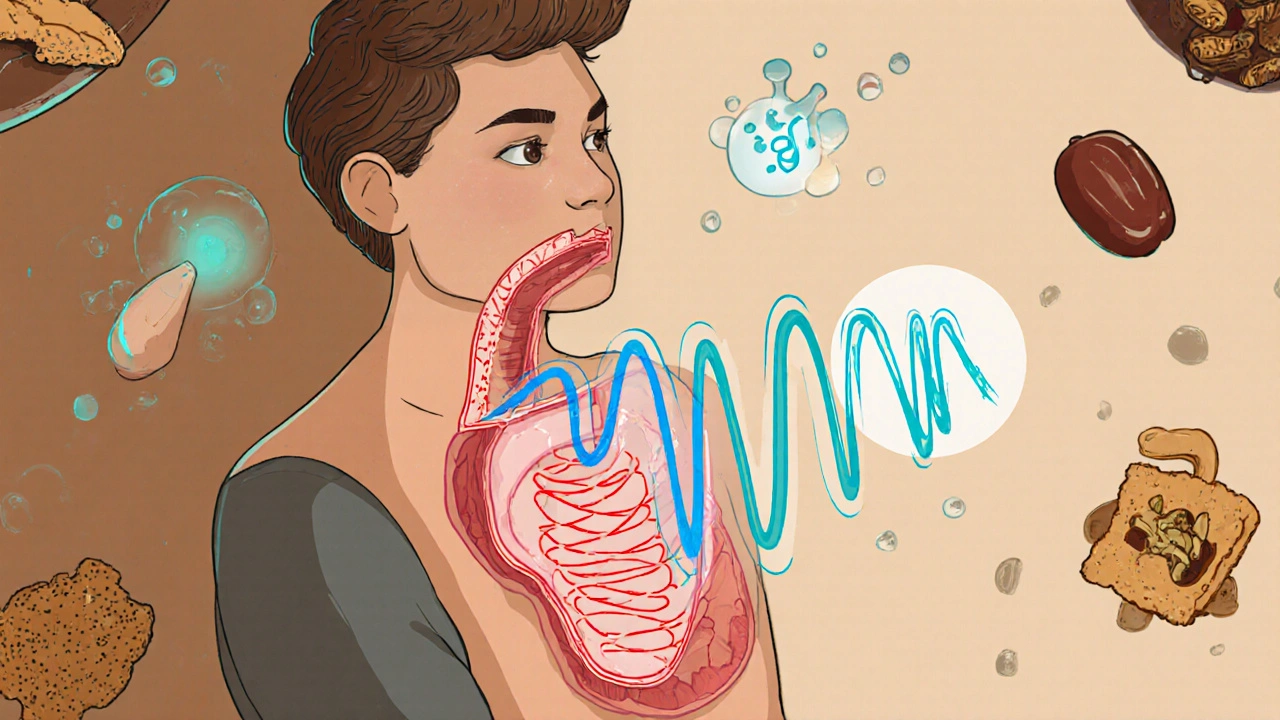
Swallowing should be easy. But for people with esophageal motility disorders, every bite can feel like a battle. Food sticks, chest pain flares up, and no matter how much you chew, it never seems to move down right. This isn’t just discomfort-it’s a disruption to daily life. Acotiamide is emerging as a targeted solution for these issues, especially when standard treatments like proton pump inhibitors fail to help. Unlike acid reducers, acotiamide works on the muscles that move food through your digestive tract, making it a game-changer for certain types of dyspepsia and esophageal dysfunction.
What is acotiamide?
Acotiamide is a prokinetic drug developed in Japan and approved for use there since 2014. It’s not a new chemical; it’s a carefully designed molecule that targets specific receptors in the gut to improve muscle coordination. Unlike older prokinetics like metoclopramide or cisapride, acotiamide doesn’t cross the blood-brain barrier. That means it avoids side effects like drowsiness, anxiety, or movement disorders-common problems with drugs that affect dopamine in the brain.
Its main action? Boosting acetylcholine release in the stomach and esophagus. Acetylcholine is the neurotransmitter that tells muscles to contract. In people with motility disorders, this signal gets weak. Acotiamide restores it. Studies show it increases the strength and frequency of contractions in the lower esophageal sphincter and improves gastric emptying. This isn’t just theory-real patients report less bloating, fewer episodes of food sticking, and better overall digestion within weeks.
How does acotiamide help esophageal motility?
Esophageal motility disorders aren’t one condition. They include things like achalasia, diffuse esophageal spasm, and esophagogastric junction outflow obstruction. Many of these are diagnosed with high-resolution manometry, which measures pressure waves as you swallow. In functional dyspepsia with esophageal involvement, the problem isn’t structural-it’s functional. The muscles don’t coordinate properly, even though scans look normal.
Acotiamide doesn’t fix anatomical blockages. Instead, it improves the timing and force of contractions in the esophagus. A 2021 randomized trial published in Gastroenterology followed 120 patients with functional dyspepsia and confirmed esophageal motility abnormalities. Those taking acotiamide (100 mg three times daily) showed a 40% improvement in esophageal peristalsis compared to placebo. Patients also reported a 50% reduction in post-meal chest pain and a significant drop in the feeling that food was stuck.
What’s more, acotiamide works quickly. Most patients notice changes in swallowing within 7 to 10 days. This is faster than many other prokinetics, which often take weeks to show benefit. For someone struggling to eat without pain, that speed matters.
Who benefits most from acotiamide?
Not everyone with indigestion needs acotiamide. It’s most effective for people with:
- Post-meal fullness and early satiety that doesn’t improve with acid blockers
- Recurrent chest pain after eating, ruled out for heart issues
- Normal endoscopy and no signs of GERD or ulcers
- Abnormal esophageal motility on manometry, especially weak or uncoordinated contractions
It’s not for people with mechanical obstructions-like a stricture or tumor-or those with severe achalasia. In those cases, dilation or surgery is still the standard. But for the growing group of patients labeled with "functional" disorders-where tests are normal but symptoms are real-acotiamide fills a critical gap.
It’s also a good option for older adults. Many prokinetics carry risks for seniors due to neurological side effects. Acotiamide’s clean profile makes it safer for this group. A 2023 Japanese study of patients over 65 found no increase in dizziness or tremors, even after 12 weeks of use.

How does it compare to other treatments?
Let’s break down how acotiamide stacks up against common alternatives:
| Treatment | Target | Speed of Effect | Common Side Effects | Best For |
|---|---|---|---|---|
| Acotiamide | Acetylcholine release in gut | 7-14 days | Mild constipation, occasional headache | Functional dyspepsia with motility issues |
| Proton Pump Inhibitors (PPIs) | Stomach acid | 2-4 weeks | Diarrhea, nutrient deficiencies, bone loss | GERD with acid symptoms |
| Metoclopramide | Dopamine blockade | 1-2 weeks | Drowsiness, restlessness, tardive dyskinesia | Severe gastroparesis (short-term) |
| Domperidone | Dopamine blockade | 1-3 weeks | Headache, dry mouth, rare heart rhythm changes | Patients avoiding CNS effects |
| Botulinum Toxin (Botox) | Relaxes sphincter | Days | Temporary weakness, need for repeat injections | Achalasia (not first-line) |
Acotiamide stands out because it doesn’t just suppress symptoms-it fixes the underlying muscle dysfunction. PPIs only reduce acid, which doesn’t help if the problem is motility. Metoclopramide works but carries neurological risks. Domperidone is safer but less effective for esophageal issues. Acotiamide is the only one that directly improves esophageal peristalsis without major safety concerns.
What’s the dosing and safety profile?
The standard dose is 100 mg taken three times a day, 30 minutes before meals. It’s available as tablets in Japan and some parts of Asia. It’s not yet approved in the U.S. or EU, but clinical trials are ongoing. In countries where it’s available, it’s typically prescribed by gastroenterologists after other treatments fail.
Safety data from over 2,000 patients shows it’s well-tolerated. The most common side effects are mild: constipation (in about 5% of users), occasional headache, and rarely, mild abdominal discomfort. No cases of QT prolongation, a dangerous heart rhythm issue linked to some other prokinetics, have been reported.
It doesn’t interact with most common medications-antidepressants, blood pressure drugs, or even anticoagulants. That makes it easier to use in patients with multiple conditions. No dose adjustments are needed for kidney or liver impairment, which is rare for gut medications.
Real-world results: What patients say
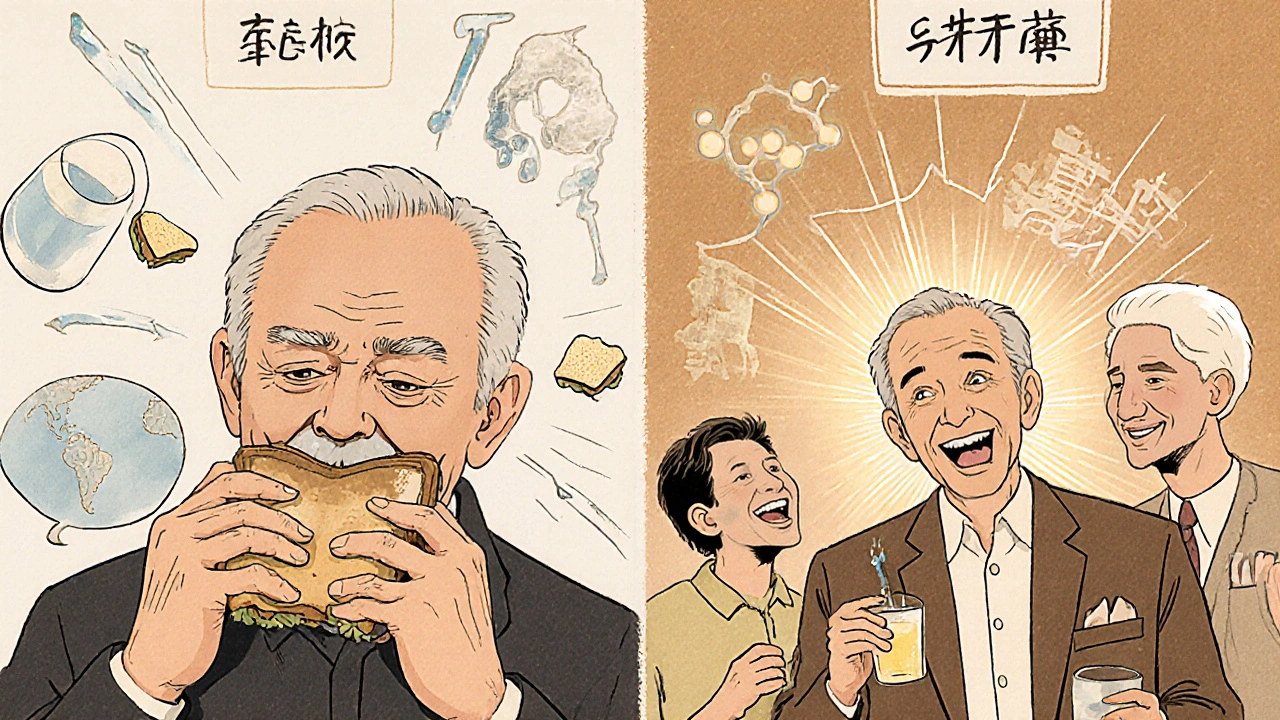
One patient, a 58-year-old teacher from Osaka, described her experience: "I used to eat lunch and then sit at my desk for an hour, afraid to move. My chest felt tight. I thought it was stress. After two weeks on acotiamide, I could swallow a sandwich without stopping. I didn’t even realize how much I’d been holding back. Now I eat with my students again."
Another, a 72-year-old retired engineer, had been told his symptoms were "just aging." He’d tried PPIs, fiber supplements, even dietary changes. Nothing worked. His doctor ordered a manometry test-it showed weak esophageal contractions. After starting acotiamide, his swallowing score improved from 2 out of 10 to 8 out of 10 in six weeks. He no longer needs to drink water with every bite.
These aren’t isolated cases. Real-world data from Japanese clinics shows that 68% of patients with functional dyspepsia and confirmed motility issues report "significant improvement" after 8 weeks on acotiamide. Only 12% discontinue due to side effects.
Where is acotiamide available?
As of 2025, acotiamide is approved and widely used in Japan, South Korea, and China. It’s also available in some Southeast Asian countries under brand names like Acozid and Acoty. In the U.S. and Europe, it’s still under review by regulatory agencies. Clinical trials are active in the U.K., Canada, and Australia, with results expected by late 2026.
Some patients travel abroad to access it, or order it through licensed international pharmacies. But caution is key-online sellers often sell counterfeit versions. Always confirm the source and check for regulatory approval in your country.
What’s next for acotiamide?
Researchers are now studying acotiamide for other conditions linked to motility: gastroparesis in diabetes, chronic constipation, and even reflux that doesn’t respond to acid suppression. Early data suggests it may help reduce non-acid reflux episodes by improving esophageal clearance.
It’s also being tested in combination with low-dose antidepressants for patients with both motility issues and anxiety-related symptoms. The idea? Fix the physical problem while addressing the brain-gut connection.
For now, acotiamide remains a niche but powerful tool. It’s not a cure-all, but for the right person-someone with real, measurable motility problems and no structural cause-it can restore normal eating, reduce pain, and bring back quality of life.
Is acotiamide approved in the United States?
No, acotiamide is not yet approved by the FDA as of 2025. It is approved in Japan, South Korea, and China, and clinical trials are ongoing in the U.S. and Europe. Patients in the U.S. may access it through compassionate use programs or international pharmacies, but only under medical supervision.
How long does it take for acotiamide to work?
Most patients notice improvement in swallowing and post-meal fullness within 7 to 14 days. Full benefit, especially in esophageal motility, typically takes 4 to 6 weeks of consistent use. It’s not a fast-acting painkiller-it’s a muscle-coordinating drug, so results build over time.
Can I take acotiamide with my other medications?
Yes, acotiamide has very few drug interactions. It doesn’t affect liver enzymes that break down most common medications like blood pressure drugs, statins, or antidepressants. Always tell your doctor what you’re taking, but there’s no need to avoid most prescriptions. It’s also safe with over-the-counter antacids.
Does acotiamide help with acid reflux?
It doesn’t reduce stomach acid, so it won’t help if your reflux is caused by too much acid. But if your reflux is due to poor esophageal clearing or weak lower sphincter contractions, acotiamide can help by improving how fast food and fluid move through the esophagus. This reduces non-acid reflux episodes, which many patients experience even when PPIs don’t work.
Are there any long-term risks with acotiamide?
So far, no long-term risks have been identified in studies lasting up to two years. Unlike older prokinetics, it doesn’t cause movement disorders or heart rhythm problems. The most common issue is mild constipation, which usually resolves with increased water or fiber intake. Regular check-ins with your doctor are still recommended, especially if you’re using it for more than 6 months.
If you’ve been told your swallowing problems are "just functional" and no one has a solution, acotiamide might be worth discussing. It’s not magic-but for the right person, it’s the missing piece.

Bart Capoen
October 28, 2025 AT 21:17Jen Taylor
October 29, 2025 AT 10:23Raj Modi
October 29, 2025 AT 21:40luna dream
October 31, 2025 AT 18:27Sarah Schmidt
November 2, 2025 AT 13:31Billy Gambino
November 3, 2025 AT 04:53Christy Tomerlin
November 4, 2025 AT 07:22Susan Karabin
November 5, 2025 AT 14:04Cecil Mays
November 7, 2025 AT 02:54Karen Werling
November 8, 2025 AT 09:02Patrick Dwyer
November 9, 2025 AT 08:00Emil Tompkins
November 10, 2025 AT 23:21STEVEN SHELLEY
November 11, 2025 AT 22:57Shilah Lala
November 11, 2025 AT 23:35Linda Patterson
November 13, 2025 AT 01:44